Abstracts
Background/objectives
Obesity, defined by body mass index (BMI), is a well-known risk factor for the severity of coronavirus disease 2019 (COVID-19). Adipose tissue distribution has also been implicated as an important factor in the body’s response to infection, and excess visceral fat (VF), which is prevalent in Japanese, may contribute significantly to the severity. Therefore, this study aimed to evaluate the association of obesity and VF with COVID-19 severe illness in Japan.
Subjects/methods
This retrospective cohort study involved 550 COVID-19 patients admitted to a tertiary care hospital with BMI and body composition data, including VF. The primary endpoint was severe illness, including death, due to COVID-19 during hospitalization. Logistic regression analysis was applied to examine the quartiles of BMI and VF on severe illness after adjusting for covariates such as age, sex, subcutaneous fat, paraspinal muscle radiodensity, and comorbidities affecting VF (COPD, cancer within 5 years, immunosuppressive agent use).
Results
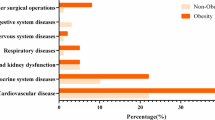
The median age was 56.0 years; 71.8% were males. During hospitalization, 82 (14.9%) experienced COVID-19 severe illness. In the multivariate logistic regression analysis, Q4 of BMI was not significantly associated with severe illness compared to Q1 of BMI (OR 1.03; 95% CI 0.37–2.86; p = 0.95). Conversely, Q3 and Q4 of VF showed a higher risk for severe illness compared to Q1 of VF (OR 2.68; 95% CI 1.01–7.11; p = 0.04, OR 3.66; 95% CI 1.30–10.26; p = 0.01, respectively). Stratified analysis by BMI and adjusted for covariates showed the positive association of VF with severe illness only in the BMI < 25 kg/m2 group.
Conclusions
High BMI was not an independent risk factor for COVID-19 severe illness in hospitalized patients in Japan, whereas excess VF significantly influenced severe illness, especially in patients with a BMI < 25 kg/m2.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
Data availability
The datasets generated and analyzed in this study are available from the corresponding author upon reasonable request.
References
Guan WJ, Ni ZY, Hu Y, Liang WH, Ou CQ, He JX, et al. Clinical characteristics of coronavirus disease 2019 in China. N Engl J Med. 2020;382:1708–20.
Wu Z, McGoogan JM. Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China: summary of a report of 72 314 cases from the Chinese Center for Disease Control and Prevention. JAMA. 2020;323:1239–42.
Mahamat-Saleh Y, Fiolet T, Rebeaud ME, Mulot M, Guihur A, El Fatouhi D, et al. Diabetes, hypertension, body mass index, smoking and COVID-19-related mortality: a systematic review and meta-analysis of observational studies. BMJ Open. 2021;11:e052777.
Du Y, Lv Y, Zha W, Zhou N, Hong X. Association of body mass index (BMI) with critical COVID-19 and in-hospital mortality: a dose-response meta-analysis. Metab Clin Exp. 2021;117:154373.
Aghili SMM, Ebrahimpur M, Arjmand B, Shadman Z, Pejman Sani M, Qorbani M, et al. Obesity in COVID-19 era, implications for mechanisms, comorbidities, and prognosis: a review and meta-analysis. Int J Obes (2005). 2021;45:998–1016.
Raeisi T, Mozaffari H, Sepehri N, Darand M, Razi B, Garousi N, et al. The negative impact of obesity on the occurrence and prognosis of the 2019 novel coronavirus (COVID-19) disease: a systematic review and meta-analysis. Eat Weight Disord. 2022;27:893–911.
Pranata R, Lim MA, Yonas E, Vania R, Lukito AA, Siswanto BB, et al. Body mass index and outcome in patients with COVID-19: a dose-response meta-analysis. Diab Metab. 2021;47:101178.
Pisitsak C, Lee JG, Boyd JH, Coxson HO, Russell JA, Walley KR. Increased ratio of visceral to subcutaneous adipose tissue in septic patients is associated with adverse outcome. Crit Care Med. 2016;44:1966–73.
Krams IA, Luoto S, Rantala MJ, Jõers P, Krama T. Covid-19: fat, obesity, inflammation, ethnicity, and sex differences. Pathogens (Basel, Switzerland). 2020;9:887.
Favre G, Legueult K, Pradier C, Raffaelli C, Ichai C, Iannelli A, et al. Visceral fat is associated to the severity of COVID-19. Metabolism. 2021;115:154440.
Tilg H, Moschen AR. Adipocytokines: mediators linking adipose tissue, inflammation and immunity. Nat Rev Immunol. 2006;6:772–83.
Tran TT, Yamamoto Y, Gesta S, Kahn CR. Beneficial effects of subcutaneous fat transplantation on metabolism. Cell Metab. 2008;7:410–20.
Chait A, den Hartigh LJ. Adipose tissue distribution, inflammation and its metabolic consequences, including diabetes and cardiovascular disease. Front Cardiovasc Med. 2020;7:22.
Feng Z, Zhao H, Kang W, Liu Q, Wu J, Bragazzi NL, et al. Association of paraspinal muscle measurements on chest computed tomography with clinical outcomes in patients with severe coronavirus disease 2019. J Gerontol Ser A Biol Sci Med Sci. 2021;76:e78–84.
Pinto FCS, Andrade MF, Gatti da Silva GH, Faiad JZ, Barrére APN, Gonçalves RC, et al. Function over mass: a meta-analysis on the importance of skeletal muscle quality in COVID-19 patients. Front Nutr. 2022;9:837719.
Yang Y, Ding L, Zou X, Shen Y, Hu D, Hu X, et al. Visceral adiposity and high intramuscular fat deposition independently predict critical illness in patients with SARS-CoV-2. Obesity (Silver Spring, MD). 2020;28:2040–8.
McGovern J, Dolan R, Richards C, Laird BJ, McMillan DC, Maguire D. Relation between body composition, systemic inflammatory response, and clinical outcomes in patients admitted to an urban teaching hospital with COVID-19. J Nutr. 2021;151:2236–44.
Pranata R, Lim MA, Huang I, Yonas E, Henrina J, Vania R, et al. Visceral adiposity, subcutaneous adiposity, and severe coronavirus disease-2019 (COVID-19): Systematic review and meta-analysis. Clin Nutr ESPEN. 2021;43:163–8.
Ogata H, Mori M, Jingushi Y, Matsuzaki H, Katahira K, Ishimatsu A, et al. Impact of visceral fat on the prognosis of coronavirus disease 2019: an observational cohort study. BMC Infect Dis. 2021;21:1240.
Organization for Economic Co-operation and Development. The heavy burden of obesity. Prevalence of obesity and morbid obesity in adults in 2016. https://www.oecd-ilibrary.org/social-issues-migration-health/prevalence-of-obesity-and-morbid-obesity-in-adults-in-2016_247a1065-en. Accessed 5 Jun 2022.
Ministry of Health, Labor and Welfare. The National Health and Nutrition Survey 2019. Distribution of abdominal circumference. https://www.e-stat.go.jp/stat-search/files. Accessed 5 Jun 2022.
Földi M, Farkas N, Kiss S, Dembrovszky F, Szakács Z, Balaskó M, et al. Visceral adiposity elevates the risk of critical condition in COVID-19: a systematic review and meta-analysis. Obesity (Silver Spring, Md). 2021;29:521–8.
Japan Society for the Study of Obesity. Guidelines for the Management of Obesity Disease 2016. Tokyo: Life Science Publishing Company; 2016.
Terada M, Ohtsu H, Saito S, Hayakawa K, Tsuzuki S, Asai Y, et al. Risk factors for severity on admission and the disease progression during hospitalisation in a large cohort of patients with COVID-19 in Japan. BMJ Open. 2021;11:e047007.
Takahashi M, Fujioka T, Horii T, Kimura K, Kimura M, Hashimoto Y, et al. Can deep learning-based volumetric analysis predict oxygen demand increase in patients with COVID-19 pneumonia? Medicina (Kaunas, Lithuania). 2021;57:1148.
Arru C, Ebrahimian S, Falaschi Z, Hansen JV, Pasche A, Lyhne MD, et al. Comparison of deep learning, radiomics and subjective assessment of chest CT findings in SARS-CoV-2 pneumonia. Clin Imaging. 2021;80:58–66.
Ofenheimer A, Breyer-Kohansal R, Hartl S, Burghuber OC, Krach F, Schrott A, et al. Reference values of body composition parameters and visceral adipose tissue (VAT) by DXA in adults aged 18-81 years-results from the LEAD cohort. Eur J Clin Nutr. 2020;74:1181–91.
Palmer BF, Clegg DJ. The sexual dimorphism of obesity. Mol Cell Endocrinol. 2015;402:113–9.
Whitworth JA, Williamson PM, Mangos G, Kelly JJ. Cardiovascular consequences of cortisol excess. Vasc Health Risk Manag. 2005;1:291–9.
Popkin BM, Du S, Green WD, Beck MA, Algaith T, Herbst CH, et al. Individuals with obesity and COVID-19: A global perspective on the epidemiology and biological relationships. Obesity Rev. 2020;21:e13128.
Chu Y, Yang J, Shi J, Zhang P, Wang X. Obesity is associated with increased severity of disease in COVID-19 pneumonia: a systematic review and meta-analysis. Eur J Med Res. 2020;25:64.
WHO Expert Consultation. Appropriate body-mass index for Asian populations and its implications for policy and intervention strategies. Lancet (London, England). 2004;363:157–63.
Goehler A, Hsu TH, Seiglie JA, Siedner MJ, Lo J, Triant V, et al. Visceral adiposity and severe COVID-19 disease: application of an artificial intelligence algorithm to improve clinical risk prediction. Open Forum Infect Dis. 2021;8:ofab275.
Kim JY, van de Wall E, Laplante M, Azzara A, Trujillo ME, Hofmann SM, et al. Obesity-associated improvements in metabolic profile through expansion of adipose tissue. J Clin Investig. 2007;117:2621–37.
Miyazaki Y, Mahankali A, Matsuda M, Mahankali S, Hardies J, Cusi K, et al. Effect of pioglitazone on abdominal fat distribution and insulin sensitivity in type 2 diabetic patients. J Clin Endocrinol Metab. 2002;87:2784–91.
Francisco V, Pino J, Campos-Cabaleiro V, Ruiz-Fernández C, Mera A, Gonzalez-Gay MA, et al. Obesity, fat mass and immune system: role for leptin. Front Physiol. 2018;9:640.
Nishimura S, Manabe I, Nagai R. Adipose tissue inflammation in obesity and metabolic syndrome. Discov Med. 2009;8:55–60.
Fontana L, Eagon JC, Trujillo ME, Scherer PE, Klein S. Visceral fat adipokine secretion is associated with systemic inflammation in obese humans. Diabetes. 2007;56:1010–3.
Finelli C. Obesity, COVID-19 and immunotherapy: the complex relationship! Immunotherapy. 2020;12:1105–9.
Conti P, Caraffa A, Tetè G, Gallenga CE, Ross R, Kritas SK, et al. Mast cells activated by SARS-CoV-2 release histamine which increases IL-1 levels causing cytokine storm and inflammatory reaction in COVID-19. J Biol Regulat Homeostat Agent. 2020;34:1629–32.
Pasquarelli-do-Nascimento G, Braz-de-Melo HA, Faria SS, Santos IO, Kobinger GP, Magalhães KG. Hypercoagulopathy and adipose tissue exacerbated inflammation may explain higher mortality in COVID-19 patients with obesity. Front Endocrinol. 2020;11:530.
Vilahur G, Ben-Aicha S, Badimon L. New insights into the role of adipose tissue in thrombosis. Cardiovasc Res. 2017;113:1046–54.
Chen L, Sun X, Han D, Zhong J, Zhang H, Zheng L. Visceral adipose tissue and risk of COVID-19 susceptibility, hospitalization, and severity: a Mendelian randomization study. Front Public Health. 2022;10:1023935.
Aubrey J, Esfandiari N, Baracos VE, Buteau FA, Frenette J, Putman CT, et al. Measurement of skeletal muscle radiation attenuation and basis of its biological variation. Acta Physiolo (Oxford, England). 2014;210:489–97.
Kuk JL, Church TS, Blair SN, Ross R. Does measurement site for visceral and abdominal subcutaneous adipose tissue alter associations with the metabolic syndrome? Diabetes Care. 2006;29:679–84.
Acknowledgements
The authors thank everyone who provides medical care to our COVID-19 patients. We especially acknowledge the following radiological technologists at the Department of Diagnostic Radiology and Nuclear Medicine, Tokyo Medical and Dental University: Hiroto Hada, Ryosuke Kaho, Kohei Maehara, Takuya Watanabe, Takumi Hiraishi, and Kosuke Inoue, for contributing to the collection and analysis of CT images.
Author information
Authors and Affiliations
Contributions
YG and TF conceived and designed this study. All authors collected the data, and YG, YN, and TF analyzed the data statistically. YG wrote the first draft of the manuscript. All authors interpreted the results and revised the content critically. They all approved the final version for submission. TF supervised the entire work and is the guarantor.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Goto, Y., Nagamine, Y., Hanafusa, M. et al. Association of excess visceral fat and severe illness in hospitalized COVID-19 patients in Japan: a retrospective cohort study. Int J Obes 48, 674–682 (2024). https://doi.org/10.1038/s41366-024-01464-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41366-024-01464-z