Abstract
Surfactant replacement therapy is currently approved by the United States Food and Drug Administration (FDA) for premature infants with respiratory distress syndrome (RDS) caused by surfactant deficiency due to immaturity. There is strong evidence that surfactant decreases mortality and air leak syndromes in premature infants with RDS. However, surfactant is also used “off-label” for respiratory failure beyond classic RDS. This review discusses current evidence for the use of off-label surfactant therapy for (1) term infants with lung disease such as meconium aspiration syndrome (MAS), pneumonia/sepsis, and congenital diaphragmatic hernia (2) premature infants after 72 h for acute respiratory failure, and (3) the use of surfactant lavage. At last, we briefly describe the use of surfactants for drug delivery and the current evidence on evaluating infants for surfactant deficiency.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
Avery ME, Mead J. Surface properties in relation to atelectasis and hyaline membrane disease. AMA J Dis Child. 1959;97:517–23.
Kallapur SG, Jobe AH Lung Development and Maturation. In: Martin RJ, Fanaroff AAWMC (eds). Fanaroff and Martin’s Neonatal-Perinatal Medicine, 2-Volume Set. Elsevier Inc., 2020, pp 1124-42.
Fujiwara T, Maeta H, Chida S, Morita T, Watabe Y, Abe T. Artificial surfactant therapy in hyaline-membrane disease. Lancet. 1980;1:55–9.
Wrobel S. Bubbles, Babies and Biology: The Story of Surfactant. FASEB J 2004; 18. https://doi.org/10.1096/fj.04-2077bkt.
Polin RA, Carlo WA, Papile L-A, Polin RA, Carlo W, Tan R, et al. Surfactant replacement therapy for preterm and term neonates with respiratory distress. Pediatrics. 2014;133:156–63.
Soll R, Blanco F. Natural surfactant extract versus synthetic surfactant for neonatal respiratory distress syndrome. In: Soll R (ed). Cochrane Database of Systematic Reviews. https://doi.org/10.1002/14651858.CD000144 John Wiley & Sons, Ltd: Chichester, UK, 2001.
Moya F, Javier MC. Myth: All surfactants are alike. Semin Fetal Neonatal Med. 2011;16:269–74.
Sweet DG, Carnielli VP, Greisen G, Hallman M, Klebermass-Schrehof K, Ozek E, et al. European Consensus Guidelines on the Management of Respiratory Distress Syndrome: 2022 Update. Neonatology. 2023;120:3–23.
Ardell S, Pfister RH, Soll R. Animal derived surfactant extract versus protein free synthetic surfactant for the prevention and treatment of respiratory distress syndrome. Cochrane Database Syst Rev. 2015;8:CD000144.
Katz LA, Klein JM. Repeat surfactant therapy for postsurfactant slump. J Perinatol. 2006;26:414–22.
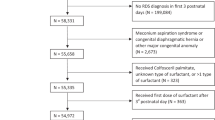
Greenberg JM, Poindexter BB, Shaw PA, Bellamy SL, Keller RL, Moore PE, et al. Respiratory medication use in extremely premature (<29 weeks) infants during initial NICU hospitalization: Results from the prematurity and respiratory outcomes program. Pediatr Pulmonol. 2020;55:360–8.
Ramaswamy VV, Abiramalatha T, Bandyopadhyay T, Boyle E, Roehr CC. Surfactant therapy in late preterm and term neonates with respiratory distress syndrome: a systematic review and meta-analysis. Arch Dis Child Fetal Neonatal Ed. 2022;107:393–7.
Roberts D, Dalziel SR. Antenatal corticosteroids for accelerating fetal lung maturation for women at risk of preterm birth. In: Roberts D (ed). Cochrane Database of Systematic Reviews. https://doi.org/10.1002/14651858.CD004454.pub2 John Wiley & Sons, Ltd: Chichester, UK, 2006.
Piper JM, Xenakis EM, Langer O. Delayed appearance of pulmonary maturation markers is associated with poor glucose control in diabetic pregnancies. J Matern Fetal Med. 1998;7:148–53.
Auten RL, Notter RH, Kendig JW, Davis JM, Shapiro DL. Surfactant treatment of full-term newborns with respiratory failure. Pediatrics. 1991;87:101–7.
Hintz SR, Suttner DM, Sheehan AM, Rhine WD, Van Meurs KP. Decreased use of neonatal Extracorporeal Membrane Oxygenation (ECMO): How new treatment modalities have affected ECMO utilization. Pediatrics. 2000;106:1339–43.
Dargaville PA. Respiratory support in meconium aspiration syndrome: a practical guide. Int J Pediatr. 2012;2012:1–9.
Olicker AL, Raffay TM, Ryan RM. Neonatal respiratory distress secondary to meconium aspiration syndrome. Children. 2021;8:246.
Sun B, Herting E, Curstedt T, Robertson B. Exogenous surfactant improves lung compliance and oxygenation in adult rats with meconium aspiration. J Appl Physiol. 1994;77:1961–71.
Sun B, Curstedt T, Song G-W, Robertson B. Surfactant improves lung function and morphology in newborn rabbits with meconium aspiration. Neonatology. 1993;63:96–104.
Moses D, Holm BA, Spitale P, Liu M, Enhorning G. Inhibition of pulmonary surfactant function by meconium. Am J Obstet Gynecol. 1991;164:477–81.
Herting E, Rauprich P, Stichtenoth G, Walter G, Johansson J, Robertson B. Resistance of different surfactant preparations to inactivation by Meconium. Pediatr Res. 2001;50:44–49.
Halliday HL, Speer CP, Robertson B. Treatment of severe meconium aspiration syndrome with porcine surfactant. Eur J Pediatr. 1996;155:1047–51.
Findlay RD, Taeusch HW, Walther FJ. Surfactant replacement therapy for meconium aspiration syndrome. Pediatrics. 1996;97:48–52.
Lotze A, Mitchell BR, Bulas DI, Zola EM, Shalwitz RA, Gunkel JH. Multicenter study of surfactant (beractant) use in the treatment of term infants with severe respiratory failure. J Pediatr. 1998;132:40–47.
Chinese Collaborative Study Group for Neonatal Respiratory Diseases. Treatment of severe meconium aspiration syndrome with porcine surfactant: a multicentre, randomized, controlled trial. Acta Paediatr. 2005;94:896–902.
Konduri GG, Lakshminrusimha S. Surf early to higher tides: surfactant therapy to optimize tidal volume, lung recruitment, and iNO response. J Perinatol. 2021;41:1–3.
El Shahed AI, Dargaville PA, Ohlsson A, Soll R. Surfactant for meconium aspiration syndrome in term and late preterm infants. Cochrane Database Syst Rev. 2014;2014:CD002054.
Mosca F, Colnaghi M, Castoldi F. Lung lavage with a saline volume similar to functional residual capacity followed by surfactant administration in newborns with severe meconium aspiration syndrome. Intensive Care Med. 1996;22:1412–3.
Wiswell TE, Knight GR, Finer NN, Donn SM, Desai H, Walsh WF, et al. A multicenter, randomized, controlled trial comparing Surfaxin (Lucinactant) lavage with standard care for treatment of meconium aspiration syndrome. Pediatrics. 2002;109:1081–7.
Dargaville PA, Copnell B, Mills JF, Haron I, Lee JKF, Tingay DG, et al. Randomized controlled trial of lung lavage with dilute surfactant for meconium aspiration syndrome. J Pediatr 2011; 158. https://doi.org/10.1016/j.jpeds.2010.08.044.
Dargaville PA. Innovation in surfactant therapy I: Surfactant lavage and surfactant administration by fluid bolus using minimally invasive techniques. Neonatology 2012;101:326–36.
Arayici S, Sari FN, Kadioglu Simsek G, Yarci E, Alyamac Dizdar E, Uras N, et al. Lung lavage with dilute surfactant vs. bolus surfactant for meconium aspiration syndrome. J Trop Pediatr. 2019;65:491–7.
Fuchimukai T, Fujiwara T, Takahashi A, Enhorning G. Artificial pulmonary surfactant inhibited by proteins. J Appl Physiol. 1987;62:429–37.
Herting E, Gefeller O, Land M, van Sonderen L, Harms K, Robertson B. Surfactant treatment of neonates with respiratory failure and Group B Streptococcal infection. Pediatrics. 2000;106:957–64.
Deshpande S. Surfactant therapy for early onset pneumonia in late preterm and term neonates needing mechanical ventilation. J Clin Diagn Res. https://doi.org/10.7860/JCDR/2017/28523.10520 2017.
Rong Z, Mo L, Pan R, Zhu X, Cheng H, Li M, et al. Bovine surfactant in the treatment of pneumonia-induced–neonatal acute respiratory distress syndrome (NARDS) in neonates beyond 34 weeks of gestation: a multicentre, randomized, assessor-blinded, placebo-controlled trial. Eur J Pediatr. 2021;180:1107–15.
González A, Bancalari A, Osorio W, Luco M, González A, Pérez H, et al. Early use of combined exogenous surfactant and inhaled nitric oxide reduces treatment failure in persistent pulmonary hypertension of the newborn: a randomized controlled trial. J Perinatol. 2021;41:32–38.
Hansmann G, Koestenberger M, Alastalo T-P, Apitz C, Austin ED, Bonnet D, et al. 2019 updated consensus statement on the diagnosis and treatment of pediatric pulmonary hypertension: The European Pediatric Pulmonary Vascular Disease Network (EPPVDN), endorsed by AEPC, ESPR and ISHLT. J Heart Lung Transplant. 2019;38:879–901.
Willson DF, Truwit JD, Conaway MR, Traul CS, Egan EE. The adult calfactant in acute respiratory distress syndrome trial. Chest. 2015;148:356–64.
Spragg RG, Lewis JF, Walmrath H-D, Johannigman J, Bellingan G, Laterre P-F, et al. Effect of recombinant surfactant protein C–based surfactant on the acute respiratory distress syndrome. N. Engl J Med. 2004;351:884–92.
Meng S-S, Chang W, Lu Z-H, Xie J-F, Qiu H-B, Yang Y, et al. Effect of surfactant administration on outcomes of adult patients in acute respiratory distress syndrome: a meta-analysis of randomized controlled trials. BMC Pulm Med. 2019;19:9.
Spragg RG, Taut FJH, Lewis JF, Schenk P, Ruppert C, Dean N, et al. Recombinant surfactant protein C-based surfactant for patients with severe direct lung injury. Am J Respir Crit Care Med. 2011;183:1055–61.
Wilcox DT, Glick PL, Karamanoukian H, Rossman J, Morin FC, Holm BA. Pathophysiology of congenital diaphragmatic hernia. V. Effect of exogenous surfactant therapy on gas exchange and lung mechanics in the lamb congenital diaphragmatic hernia model. J Pediatr. 1994;124:289–93.
Glick PL, Stannard VA, Leach CL, Rossman J, Hosada Y, Morin FC, et al. Pathophysiology of congenital diaphragmatic hernia II: the fetal lamb CDH model is surfactant deficient. J Pediatr Surg. 1992;27:382–7.
Bae CW, Jang CK, Chung SJ, Choi YM, Oh SM, Lee TS, et al. Exogenous pulmonary surfactant replacement therapy in a neonate with pulmonary hypoplasia accompanying congenital diaphragmatic hernia–a case report. J Korean Med Sci. 1996;11:265–70.
Lotze A, Knight GR, Anderson KD, Hull WM, Whitsett JA, O’Donnell RM, et al. Surfactant (beractant) therapy for infants with congenital diaphragmatic hernia on ECMO: Evidence of persistent surfactant deficiency. J Pediatr Surg. 1994;29:407–12.
Van Meurs K. Is surfactant therapy beneficial in the treatment of the term newborn infant with congenital diaphragmatic hernia? J Pediatr. 2004;145:312–6.
Sobel DB, Carroll A. Postsurfactant slump: early prediction of neonatal chronic lung disease? J Perinatol. 1994;14:268–74.
Attar MA, Donn SM. Mechanisms of ventilator-induced lung injury in premature infants. Semin Neonatol. 2002;7:353–60.
Laughon M, Bose C, Moya F, Aschner J, Donn SM, Morabito C, et al. A pilot randomized, controlled trial of later treatment with a peptide-containing, synthetic surfactant for the prevention of bronchopulmonary dysplasia. Pediatrics. 2009;123:89–96.
Hascoët J-M, Picaud J-C, Ligi I, Blanc T, Moreau F, Pinturier M-F, et al. Late surfactant administration in very preterm neonates with prolonged respiratory distress and pulmonary outcome at 1 year of age. JAMA Pediatr. 2016;170:365.
Ballard RA, Keller RL, Black DM, Ballard PL, Merrill JD, Eichenwald EC, et al. Randomized trial of late surfactant treatment in ventilated preterm infants receiving inhaled nitric oxide. J Pediatrics. 2016;168:23–29.e4.
Pandit PB, Dunn MS, Kelly EN, Perlman M. Surfactant replacement in neonates with early chronic lung disease. Pediatrics. 1995;95:851–4.
Lane MD, Kishnani S, Udemadu O, Danquah SE, Treadway RM, Langman A, et al. Comparative efficacy and safety of late surfactant preparations: a retrospective study. J Perinatol. 2021;41:2639–44.
Keller RL, Eichenwald EC, Hibbs AM, Rogers EE, Wai KC, Black DM, et al. The randomized, controlled trial of late surfactant: effects on respiratory outcomes at 1-year corrected age. J Pediatr. 2017;183:19–25.e2.
Keller RL, Merrill JD, Black DM, Steinhorn RH, Eichenwald EC, Durand DJ, et al. Late administration of surfactant replacement therapy increases surfactant protein-B content: a randomized pilot study. Pediatr Res. 2012;72:613–9.
Merrill JD, Ballard RA, Cnaan A, Hibbs AM, Godinez RI, Godinez MH, et al. Dysfunction of pulmonary surfactant in chronically ventilated premature infants. Pediatr Res. 2004;56:918–26.
Beauchene MS, Cunningham AM, Stanford AH, Bischoff AR, Dagle JM, Rios DR, et al. Patent ductus arteriosus (PDA) and response to late surfactant treatment in premature infants. J Perinatol. 2023;43:1245–51.
O’Brodovich HM, Weitz JI, Possmayer F. Effect of Fibrinogen degradation products and lung ground substance on surfactant function. Neonatology. 1990;57:325–33.
Holm BA, Notter RH. Effects of hemoglobin and cell membrane lipids on pulmonary surfactant activity. J Appl Physiol. 1987;63:1434–42.
Aziz A, Ohlsson A. Surfactant for pulmonary haemorrhage in neonates. Cochrane Database Syst Rev. 2020;2:CD005254.
Pandit PB, Dunn MS, Colucci EA. Surfactant therapy in neonates with respiratory deterioration due to pulmonary hemorrhage. Pediatrics. 1995;95:32–6.
Amizuka T, Shimizu H, Niida Y, Ogawa Y. Surfactant therapy in neonates with respiratory failure due to haemorrhagic pulmonary oedema. Eur J Pediatr. 2003;162:697–702.
Thébaud B, Goss KN, Laughon M, Whitsett JA, Abman SH, Steinhorn RH, et al. Bronchopulmonary dysplasia. Nat Rev Dis Prim. 2019;5:78.
Doyle LW, Halliday HL, Ehrenkranz RA, Davis PG, Sinclair JC. An update on the impact of postnatal systemic corticosteroids on mortality and cerebral palsy in preterm infants: effect modification by risk of bronchopulmonary dysplasia. J Pediatr. 2014;165:1258–60.
Watterberg KL. American Academy of Pediatrics. Committee on Fetus and Newborn. Policy statement–postnatal corticosteroids to prevent or treat bronchopulmonary dysplasia. Pediatrics. 2010;126:800–8.
Yeh TF, Chen CM, Wu SY, Husan Z, Li TC, Hsieh WS, et al. Intratracheal administration of Budesonide/surfactant to prevent Bronchopulmonary Dysplasia. Am J Respir Crit Care Med. 2016;193:86–95.
Kothe TB, Sadiq FH, Burleyson N, Williams HL, Anderson C, Hillman NH. Surfactant and budesonide for respiratory distress syndrome: an observational study. Pediatr Res. 2020;87:940–5.
Manley BJ, Kamlin COF, Donath S, Huang L, Birch P, Cheong JLY, et al. Intratracheal budesonide mixed with surfactant to increase survival free of bronchopulmonary dysplasia in extremely preterm infants: study protocol for the international, multicenter, randomized PLUSS trial. https://doi.org/10.1186/s13063-023-07257-5 2023.
Bhandari V, Black R, Gandhi B, Hogue S, Kakkilaya V, Mikhael M, et al. RDS-NExT workshop: consensus statements for the use of surfactant in preterm neonates with RDS. J Perinatol. 2023;43:982–90.
Taylor G, Jackson W, Hornik CP, Koss A, Mantena S, Homsley K, et al. Surfactant administration in preterm infants: drug development opportunities. J Pediatr. 2019;208:163–8.
Fiori HH, Henn R, Baldisserotto M, Bica IGO, Fiori RM. Evaluation of surfactant function at birth determined by the stable microbubble test in term and near term infants with respiratory distress. Eur J Pediatr. 2004;163:443–8.
Teeratakulpisarn J, Taksaphan S, Pengsaa K, Wiangnon S, Kosuwon W. Prediction of idiopathic respiratory distress syndrome by the stable microbubble test on gastric aspirate. Pediatr Pulmonol. 1998;25:383–9.
Bhuta T, Kent-Biggs J, Jeffery HE. Prediction of surfactant dysfunction in term infants by the click test. Pediatr Pulmonol. 1997;23:287–91.
Verder H, Ebbesen F, Linderholm B, Robertson B, Eschen C, Arrøe M, et al. Prediction of respiratory distress syndrome by the microbubble stability test on gastric aspirates in newborns of less than 32 weeks’ gestation. Acta Paediatr. 2003;92:728–33.
Autilio C, Echaide M, Benachi A, Marfaing-Koka A, Capoluongo ED, Pérez-Gil J, et al. A noninvasive surfactant adsorption test predicting the need for surfactant therapy in preterm infants treated with continuous positive airway pressure. J Pediatr. 2017;182:66–73.e1.
Ravasio A, Cruz A, Pérez-Gil J, Haller T. High-throughput evaluation of pulmonary surfactant adsorption and surface film formation. J Lipid Res. 2008;49:2479–88.
Funding
The authors declare no external funding.
Author information
Authors and Affiliations
Contributions
RMR provided the leadership, senior directorship, and the review outline and concept. HA, RKD and SL contributed to the drafting, reviewing, and revision of the manuscript. All authors approved the final manuscript as submitted and agreed to be accountable for all aspects of the work. SL contributed the figures.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Desai, R.K., Yildiz Atar, H., Lakshminrusimha, S. et al. Use of surfactant beyond respiratory distress syndrome, what is the evidence?. J Perinatol 44, 478–487 (2024). https://doi.org/10.1038/s41372-024-01921-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41372-024-01921-7