Abstract
Objective
To determine the prevalence of eating disorders and orthorexia in postpartum women and examine the relationship with postpartum depression.
Study design
Included in this study were 227 postpartum women. The Eating Attitude Test-26 (EAT-26) was used to determine the risk of eating disorders in the women, followed by the Orthorexia 11 Scale (ORTO-11) to identify orthorexia, and the Edinburgh Postpartum Depression Scale (EPDS) to identify postpartum depression.
Results
63 of the women (27.8%) exhibited an orthorexic tendency, which was also related to eating disorders and postpartum depression. Each one-point increase in the EAT-26 score led to a decrease of 0.32 points in the ORTO-11 score. Similarly, each one-point increase in the EPDS score caused a reduction of 0.18 points in the ORTO-11 score. The ORTO-11 score increased by 0.26 points per each live birth.
Conclusion
An obsessive focus on healthful nutrition may result in the impairment of health and numerous adverse psychological and physiological outcomes in the future. Healthy eating habits should be maintained to improve the quality of life without causing an obsession with healthy eating.
Similar content being viewed by others
Introduction
Pregnancy and delivery are significant events in the human life cycle that bring about profound biological, social, and psychological changes. Eating disorders accompanying this process may have a negative impact on pregnancy, delivery, and the offspring [1, 2]. Pregnancy and the postpartum period might be vulnerable times for the development of eating disorders. Physical and body weight changes caused by pregnancy during these periods are significant events that contribute to the emergence of eating disorders in pregnant women [3].
The term “orthorexia nervosa” is defined as an unhealthy obsession with healthy eating. Orthorexic people are often obsessed with the quality of their diet rather than the amount, spending much time inspecting the source, processing, and packaging of foods that are then sold in the marketplaces. The obsession with food quality – a combination of the nutritional value of food as well its sensed purity – is caused by a craving to maximize one’s physical health and well-being, rather than pious faiths or worries about sustainable farming, ecological preservation, or animal prosperity [4]. Orthorexia nervosa has been the topic of many studies despite not being included in the American Psychiatric Association Diagnostic and Statistical Manual of Mental Disorders-V (APA DSM-V) [5]. It has also been linked to other eating disorders [6]. Eating disorders are accompanied by major rates of psychiatric disorders. While a range of disorders occur together, including bulimia nervosa, anorexia nervosa, binge-eating disorder, and other specified feeding and eating disorders, the percentages of comorbid mood and anxiety disorders are especially increased [7, 8].
Postpartum depression is a major problem for postpartum women. Its prevalence was reported to be 13% in the first meta-analysis research, which included 59 studies on postpartum depression [9]. The prevalence of postpartum depression differs in developed and developing cities in Türkiye and is estimated to be around 24% [10]. Women who have an eating disorder or anxiety about eating are at a higher risk of suffering from depression during the postpartum period [11, 12]. Women with a history of eating disorders reported higher depressive symptoms and anxiety in the postpartum period than those without it [13]. In one study, 40% of women with a history of anorexia nervosa developed depression during their pregnancy, and 35% scored higher than 12 on the Edinburgh Postpartum Depression Scale (EPDS), indicating a significant likelihood of being diagnosed with postpartum depression. Furthermore, women with bulimia nervosa and binge eating syndrome are prone to postpartum depression [12]. Postpartum depression has been reported in approximately 35% of women with a history of any eating disorders [2].
The postpartum term is a time of high risk for improving/keeping eating styles that may poorly affect mental health and well-being [14]. Kappa et al. reported that postpartum women with clinical eating disorder symptoms have lower body image satisfaction [15]. Much attention is placed on appearance in Western culture, with considerable pressures to maintain a socially acceptable weight and shape. The consequent body dissatisfaction and concern over body image and size may be related to high levels of distress and deterioration, which can contribute to dietary anxieties and eating disorders. Many women experience negative feelings about their bodies after pregnancy, making pregnancy and the postpartum period a particularly vulnerable time. These concerns are linked to several unfavorable physical and mental health outcomes in postpartum women, including eating and feeding challenges, and result from pregnancy-related physical changes that move women away from social thinness norms [16]. It is unclear whether changes in eating habits during pregnancy persist in the postpartum period. Some clinical studies have shown that the postpartum period is a high-risk time for anorexia nervosa and bulimia nervosa [17, 18]. It was reported that body image concerns may be slightly higher in the postpartum period relative to pregnancy, recommending that it may be an especially suitable time for intervention or that addressing such issues in pregnancy may help women to avoid the worsening of these problems [19].
Although many studies have revealed eating disorders in postpartum women [2, 20,21,22], there have been few studies on the relationship between eating disorders and depression in the postpartum period [12, 20, 23]. Furthermore, no studies have been carried out on the relationship between orthorexic tendency and depression in postpartum women. Especially in Türkiye, there is a big gap in the studies carried out on this subject, as the studies carried out were in Western countries. Therefore, this study aimed to investigate the effect of eating disorders and orthorexic tendency on the risk of postpartum depression, and the relationship between eating disorders, postpartum depression, and orthorexic tendency.
Materials and method
Study setting and population
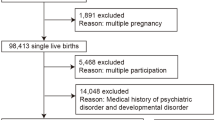
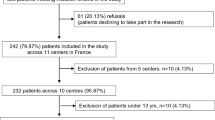
This cross-sectional study included women who applied to the Gynecology and Obstetrics Clinic at Gümüşhane State Hospital, bore a healthy birth, were over 18 years of age, and had a baby aged 0–180 days. Women with alcoholism and substance abuse, with multiple pregnancies, adolescent pregnant women, who were pregnant at the time of this study, and those with chronic or acute disease, such as kidney disease, diabetes, cancer, cardiovascular diseases, and thyroid disease, were omitted from the study.
A post-hoc power analysis was performed to establish whether the study had sufficient power. The effect size was calculated to be 0.19 based on the relationship between the risk of eating disorders and the risk of depression. Accordingly, the study’s post hoc power was calculated to be 0.59. Therefore, it was determined that there was a 59% likelihood of detecting the observed difference. The women who agreed to participate in the study signed a written consent form, and Ethics Committee approval was obtained from Gümüşhane University Ethics Committee (protocol no: 20197). The study data were gathered using a questionnaire prepared by the researchers. The women were asked to fill in the questionnaire form during a face-to-face interview, which included their general sociodemographic information (age, occupation, education level), some dietary habits (number of main and snack meals, skipped meals, most skipped meals, water consumption), some pregnant period characteristics (pregnancy plan status, whether they had a risky pregnancy, having health problems during pregnancy, gaining weight during pregnancy), Eating Attitude Test-26 (EAT-26), Orthorexia 11 Scale (ORTO-11), and Edinburgh Depression Scale. Data on some anthropometric parameters measured by the researcher were analyzed. The women also reported their height (in centimetres) and body weight (in kilograms) before their recent pregnancy. Their height and weight were used to compute the postpartum body mass index (BMI) and pre-pregnancy BMI.
Anthropometric measurements
The BMI was calculated after measuring the weight and height of women by the researcher in accordance with the methodology. The body weights were measured using a Sinbo SBS 4425 model device with 1 kg of precision on an empty stomach and while wearing thin clothing. The height was measured using the Seca height measurement instrument while the feet were together, and the head was on the Frankfurt plane. The BMI (kg/m2) was calculated by dividing the body weight (in kilograms) by the square of the height (in meters), and the resultant values were evaluated in accordance with the World Health Organization classification. This classification indicates that women with a BMI of <18.5 are underweight, those with a range of 18.5–24.9 are normal, those with a BMI of 25–29.9 are overweight, and those with a BMI of ≥30 are obese [24].
Instruments
EAT-26
The EAT-26 is a self-reported scale used by individuals. This test, developed by Garner and Garfinkel [25] for evaluating anorexia nervosa symptoms, was adapted into Turkish by Savaşır and Erol [26]. It is built on the original EAT-40 and is composed of 26 six-point Likert-type items. In this test, values ranging from 0 to 78 can be used. The EAT-26 has a cut-off point of 20 scores. Individuals with a score of 20 or more are considered to have “abnormal eating behavior,” whereas those with a score less than 20 are regarded as having “normal eating behavior” [26]. The responses are rated on a Likert scale of 1 (never) to 6 (always). Responses 4–6 are scored as 0, response 1 is scored as 3, response 2 is scored as 2, and response 3 is scored as 1, to calculate the total score. In question 25, however, responses 1, 2, and 3 are scored as 0, and responses 4, 5, and 6 are scored as 1, 2, and 3, respectively [27].
ORTO-11
The ORTO-11 is a 4-point Likert-type scale that was created through the removal of 4 questions from the ORTO-15 scale developed by Donini et al. [28] in order to detect orthorexia behaviors. Its validity and reliability were assessed by Arusoğlu et al. [29]. Always, often, sometimes, and never responses were scored as 1, 2, 3, and 4, and reverse scoring was used for question 6. The lower quartile (25%) was established by the approach used by Arusoğlu et al. [29] to determine the cut-off point, which proved to be 24. In this regard, one can say that if the scale scores are 24 or lower, there is an orthorexic tendency and if it is greater than 24, there is no orthorexic tendency. Lower scores on the ORTO-11 have been known to be associated with an orthorexic tendency.
EPDS
The EPDS is a scale designed to assess the risk and extent of postpartum depression. Developed by Cox et al. [30] in 1987, this scale was adapted into Turkish by Engindeniz et al. It is a 4-point Likert-type scale in which questions 1, 2, and 4 are scored as 0, 1, 2, 3, and the other questions are scored as 3, 2, 1, 0. On the scale, the highest points that can be obtained is 30 and the lowest is 0. The cutoff score is ≥13. If the score is 13 or higher, the subject is considered to be at risk for postpartum depression [31].
Statistical analysis
The data were analyzed using IBM SPSS Statistics for Windows 23.0 (IBM Corp., Armonk, NY, USA). The numerical data were given as the mean and standard deviation (x ± ss), while the categorical data were presented as numbers and percentages. Pearson correlation analysis was used to examine the relationship between the two groups for numerical data with a normal distribution, whereas Spearman correlation analysis was used for data with a non-normal distribution. Multiple linear regression analysis (with the ORTO-11 score as the dependent variable) was performed as well. P < 0.05 was deemed statistically significant.
Results
Of the postpartum women included in the study, 18% were primary school graduates, while 31% were university graduates. In addition, most of the participants (83%) were housewives. Their mean age was 29.7 ± 5.5 years. When asked about the plan and risk of their pregnancies, 75.3% had planned pregnancies, while 19% had risky pregnancies. When they were asked from whom they received support after delivery, 38% reported support from their spouses and 30% reported support from their mother/mother-in-law. The average number of pregnancies among women was 2.5 ± 1.2, and the average number of stillbirths or miscarriages was 1.3 ± 0.7. Their average age at first pregnancy was 23.8 ± 4.1 years. Moreover, 28% were also found to exhibit orthorexic tendency, and 16% were observed to be at risk for postpartum depression. In addition, 24% of the postpartum women were at risk for eating disorders. In regard to the BMI, 48% began their pregnancies with a normal BMI and approximately 46% were overweight and obese (Table 1).
The ORTO-11, EAT-26, and EPDS total scores were not significantly correlated with the BMI, pre-pregnancy BMI, body weight gain during pregnancy, or prepartum and postpartum body weights (P > 0.05). The correlation between the total ORTO-11 score and the education level of the postpartum women was negative (r = –0.18, P = 0.005). The Fig. 1 summarizes the relationship between the scale scores of the women by depicting a positive correlation between the EAT-26 total score and the EPDS total score (r = 0.15, P = 0.021). The Fig. 1 also demonstrates that the ORTO-11 total score was negatively correlated with both the EAT-26 (r = –0.39, P = 0.000) and the EPDS (r = –0.19, P = 0.004).
The ORTO-11 score was estimated using multiple linear regression based on (age, first gestational age, newborn age, number of live births, number of pregnancies, planned pregnancy, pre-pregnancy BMI classification and current BMI classification, EAT-26, and EPDS scores). The R2 value of 0.15 indicated a significant regression. The ORTO-11 score increased by 0.26 points per each live birth. Each one-point increase in the EAT-26 score led to a decrease of 0.32 points in the ORTO-11 score. Similarly, each one-point increase in the EPDS score caused a reduction of 0.18 points in the ORTO-11 score (Table 2).
Discussion
Although there are numerous studies on the relationship between eating disorders and depression, those on this relationship in postpartum women are limited. Moreover, no research has been conducted on the relationship between depression and orthorexia in postpartum women. Assessing the risk of eating disorders and orthorexic tendency in postpartum women and figuring out whether these factors influence the development of postpartum depression could be helpful in the development of prevention strategies for postpartum women and their newborns.
In this study, whether eating disorders and orthorexia are associated with postpartum depression among postpartum women was investigated.
Despite the fact that many women with eating disorders experience improvement and alleviation of their symptoms during pregnancy, postpartum symptoms often worsen [32]. Concerns about body weight and shape in the postpartum period may facilitate the development of malnutrition behaviors in postpartum individuals [33]. In the present study, the risk for eating disorders was 24% in the postpartum women. Cici Saraç and Bülbül [34] reported that the risk for eating disorders was 19% in postpartum women. Pettersson et al. [22] found that the prevalence of eating disorders in postpartum women was 13%. Our previous study on university students showed that the prevalence of eating disorders among female students was 14% [35]. It is possible that eating disorders are more prevalent during the postpartum period than during other periods. Therefore, awareness regarding this issue should be raised, and it can be suggested that women at risk be identified through prenatal and postpartum dietary follow-ups.
The BMI is one of the most influential factors in eating attitude [36]. In this study, only 48% of women bearing live birth began their pregnancies with a normal BMI (18.5–24.9 kg/m2). Similarly, the Center for Disease Control and Prevention stated that 49% of women possessed a normal BMI before becoming pregnant [37]. Given that being overweight or obese is associated with body dissatisfaction and this is a risk factor for eating disorders [38], dietary counseling should be provided to women during pregnancy planning, and pregnancy should be initiated with an ideal body weight.
Studies have shown that pregnant women with eating disorders gain more weight than others [39, 40]. Although there is a correlation between eating disorders and pregnancy-induced body weight gain, this was not the case in our sample. Body dissatisfaction resulting from weight gain during pregnancy and the postpartum period may lead to eating disorders in women [41]. During the postpartum period, women frequently visit health institutions for routine check-ups of their infants, and these check-ups could be an essential opportunity for evaluating maternal health, maternal concerns about body weight, and eating disorders. Determination to maintain recommended weight gain during pregnancy and optimal postpartum weight may prevent the development of eating disorders. Additionally, it may be effective in mitigating natal complications while positively impacting mother-child communication and breastfeeding behavior [41].
Although orthorexia nervosa can be described as a pathological obsession with a proper diet characterized by a restrictive diet, eating habits made according to specific rules, and strict avoidance of food believed to be unhealthy and impure, it has not yet been included as a type of eating disorder in the APA DSM-V [5, 42]. The number of studies on the prevalence of orthorexic tendency has increased in tandem with the increasing interest in this field of study. In the present study, the prevalence of orthorexic tendency was 28% in the postpartum women. Similarly, Arusoğlu [29] found that the orthorexic tendency was 27% among the female participants in a study on university employees. Similar studies on pregnant and postpartum women have yielded the following results: In their study on pregnant women admitted to the obstetrics clinics of a private hospital, Altıner and Okumuş [43] reported the prevalence of orthorexic tendency as 64%. In their study of 116 postpartum women in a private hospital, Cici Saraç and Bülbül [34] found a prevalence of 80% for orthorexic tendency. Ayhan Baser and Cankurtaran [44] reported the prevalence of orthorexic tendency as 88% in their study on 370 postpartum women. When comparing the above-mentioned studies and the present study, the largest difference between their sampling and our own was that their sampling was composed of women with higher levels of education. Thus, the rates of orthorexic tendency being higher in those studies than in the current study might be attributable to the higher educational status of the women who participated in those studies. Furthermore, the lack of a precise cut-off point for the ORTO-11 and the adoption of a distinct method for calculating a 25% cut-off point in each study may have contributed to the conflicting results.
There was a significant negative correlation between the mean ORTO-11 and EAT scores of the postpartum women (r = –0.39, P < 0.05). Each one-point increase in the EAT-26 score led to a decrease of 0.32 points in the ORTO-11 score. It can be expected that as orthorexic tendency in postpartum women increases, the risk of eating disorders would also increase. In a similar way, Arslantaş et al. [45] observed a significant negative correlation between the ORTO-11 and EAT-26 scores. Moreover, eating disorders such as anorexia nervosa and bulimia nervosa were frequently accompanied by orthorexia nervosa (28%) and maintained their increase even after treatment for eating disorders. Contrary to what has been reported, Gezer and Kabaran [46] claimed that the risk of orthorexia nervosa decreased as the eating disorder risk increased. An obsession with a healthful diet might promote postpartum women to develop eating disorders. The risk of developing an eating disorder can be prevented if one avoids this situation.
Several demographic variables have been found to be linked to orthorexia nervosa. Arusoğlu et al. [47] revealed that demographic factors such as gender, education status, age, marriage status (married or single) could influence orthorexic tendency. Additionally, having children has been reported to raise the orthorexic tendency. In the present study, it turns out that the ORTO-11 total score decreased as the educational status increased. This suggests that women with a higher level of education had greater access to information about healthy eating and were, as a result, more obsessed with their diet.
Studies have indicated that depressive symptoms emerge as a significant factor in the development of eating disorders [48, 49]. Women with current or past eating disorders have a higher prevalence of postpartum depression than women without a history of eating disorders [13]. Micali et al. [13] were the first to document that eating disorders enhance the risk of postpartum depression in postpartum women. The present study found symptoms of depression at 16% in the postpartum women. Similarly, the prevalence of postpartum depression was reported to be 17% in a meta-analysis of 58 studies [50]. Previous studies have shown that women with a history of eating disorders suffered from more depressive symptoms and felt more anxiety during and after pregnancy than women without a history of eating disorders [12, 13, 32]. Postpartum depression was observed in 50% of women who had experienced remission of eating disorders and were treated [20]. In this study, a statistically significant positive correlation was found between the EAT-26 total score and the EPDS total score, and the greater the risk of eating disorders, the greater the risk of experiencing postpartum depression. Identifying the eating disorders in postpartum women is crucial for alleviating the symptoms of postpartum depression and the possibility of remission.
There have been no studies conducted on the relationship between orthorexic tendency and postpartum depression in postpartum women. This study revealed that each one-point increase in the EPDS score caused a reduction of 0.18 points in the ORTO-11 score. Accordingly, as the orthorexic tendency increases, so does the risk of postpartum depression. Case-control studies also found that people obsessed with following a healthy diet suffer from depressed mood, anxiety, distress, and insomnia [51, 52]. Luck-Skorski et al. [53] reported that the rate of orthorexia behaviors was higher among more depressed participants. Consequently, evidence has demonstrated that orthorexia could be associated with substantial levels of tension and psychological distress. As a result, encouraging women to follow healthy dietary practices from pre-pregnancy might help them in refraining from depressive symptoms that occurred before and after pregnancy.
Limitations
The findings contain several limitations of this study. First, this survey study was cross-sectional. The survey was based on the women’s self-reporting, and thus, the data are limited to what the women choose to reveal. Neither depression nor the eating obsessions and eating disorders were clinically diagnosed. Measurements of the women’s prenatal body weights and babies were obtained based on their statements. Only mothers admitted to the Gynecology and Obstetrics Clinic of Gümüşhane State Hospital were included in this study and thus, responses cannot be generalizable to a wider postpartum population. The study did try to collect data from women of different ages and sociodemographic status, and despite that, the sample was mainly less-educated, middle-class women. Thus, the findings on eating disorders and depression in postpartum women of various sociodemographic, well-educated groups may not have been shown in the results of the present study.
Data availability
The datasets generated during and analyzed during the current study are available from the corresponding author on reasonable request.
References
Bulik CM, Von Holle A, Siega-Riz AM, Torgersen L, Lie KK, Hamer RM, et al. Birth outcomes in women with eating disorders in the Norwegian Mother and Child cohort study (MoBa). Int J Eat Disord. 2009;42:9–18.
Franko DL, Blais MA, Becker AE, Delinsky SS, Greenwood DN, Flores AT, et al. Pregnancy complications and neonatal outcomes in women with eating disorders. Am J Psychiatry. 2001;158:1461–1466.
Hendrick VC. Psychiatric disorders in pregnancy and the postpartum: principles and treatment. New Jersey: Humana Press; 2006.
Koven NS, Abry AW. The clinical basis of orthorexia nervosa: emerging perspectives. Neuropsychiatr Dis Treat. 2015;11:385–394.
APA. Diagnostic and Statistical Manual of Mental Disorders-V. 5th ed. Arlington, VA: Amerikan Psychiatric Association; 2013.
Turner PG, Lefevre CE. Instagram use is linked to increased symptoms of orthorexia nervosa. Eat Weight Disord - Stud Anorex, Bulim Obes. 2017;22:277–284.
Ulfvebrand S, Birgegard A, Norring C, Högdahl L, von Hausswolff-Juhlin Y. Psychiatric comorbidity in women and men with eating disorders results from a large clinical database. Psychiatry Res. 2015;230:294–299.
Lee MF, Madsen J, Williams SL, Browne M, Burke KJ. Differential effects of intuitive and disordered eating on physical and psychological outcomes for women with young children. Matern Child Health J. 2022;26:1–8.
O’Hara MW, Swain AM. Rates and risk of postpartum depression - a meta-analysis. Int Rev Psychiatry. 1996;8:37–54.
Özcan NK, Boyacıoğlu NE, Dinç H. Postpartum depression prevalence and risk factors in Turkey: a systematic review and meta-analysis. Arch Psychiatr Nurs. 2017;31:420–428.
Kimmel MC, Ferguson EH, Zerwas S, Bulik CM, Meltzer-Brody S. Obstetric and gynecologic problems associated with eating disorders. Int J Eat Disord. 2016;49:260–275.
Mazzeo SE, Slof-Op’t Landt MCT, Jones I, Mitchell K, Kendler KS, Neale MC, et al. Associations among postpartum depression, eating disorders, and perfectionism in a population-based sample of adult women. Int J Eat Disord. 2006;39:202–211.
Micali N, Simonoff E, Treasure J. Pregnancy and post-partum depression and anxiety in a longitudinal general population cohort: The effect of eating disorders and past depression. J Affect Disord. 2011;131:150–157.
Lee MF, Williams SL, Burke KJ. Striving for the thin ideal post-pregnancy: a cross-sectional study of intuitive eating in postpartum women. J Reprod Infant Psychol. 2020;38:127–138.
Kappa HM, Litteral JL, Keim SA, Jackson JL, Schofield KA, Crerand CE. Body image dissatisfaction, breastfeeding experiences, and self-efficacy in postpartum women with and without eating disorder symptoms. J Hum Lact. 2022;38:633–643.
Rodgers RF, O’Flynn JL, Bourdeau A, Zimmerman E. A biopsychosocial model of body image, disordered eating, and breastfeeding among postpartum women. Appetite. 2018;126:163–168.
Lacey JH, Smith G. Bulimia Nervosa. Br J Psychiatry. 1987;150:777–781.
Morgan JF, Lacey JH, Sedgwick PM. Impact of pregnancy on bulimia nervosa. Br J Psychiatry. 1999;174:135–140.
Vanderkruik R, Ellison K, Kanamori M, Freeman MP, Cohen LS, Stice E. Body dissatisfaction and disordered eating in the perinatal period: an underrecognized high-risk timeframe and the opportunity to intervene. Arch Women’s Ment Health. 2022;25:739–751.
Makino M, Yasushi M, Tsutsui S. The risk of eating disorder relapse during pregnancy and after delivery and postpartum depression among women recovered from eating disorders. BMC Pregnancy Childbirth. 2020;20:323.
Martini MG, Bramante A, Micali N. Eating Disorders in pregnancy and postpartum period. In: Percudani M, Brenna V, Pariante C (ed). Key Topics in Perinatal Mental Health. New Jersey: Cham: Springer International Publishing; 2022, 127–137.
Pettersson CB, Zandian M, Clinton D. Eating disorder symptoms pre- and postpartum. Arch Women’s Ment Health. 2016;19:675–680.
Nathina C. A guide for occupational therapist working with women with postpartum depression and eating disorders. North Dokato: University of North Dakota; 2021.
WHO. Global Database on Body Mass Index (BMI). 2020. Available from: https://www.who.int/nutrition/databases/bmi/en/
Garner DM, Garfinkel PE. The eating attitudes test: an index of the symptoms of anorexia nervosa. Psychol Med. 1979;9:273–279.
Erol N, Savaşır I. Eating attitude test: an index of anorexia nervosa symptoms. Turkish J Psychol. 1989;23:132–136.
Rivas T, Bersabé R, Jiménez M, Berrocal C. The eating attitudes test (EAT-26): reliability and validity in spanish female samples. Span J Psychol. 2010;13:1044–1056.
Donini LM, Marsili D, Graziani MP, Imbriale M, Cannella C. Orthorexia nervosa: a preliminary study with a proposal for diagnosis and an attempt to measure the dimension of the phenomenon. Eat Weight Disord. 2004;9:151–157.
Arusoğlu G, Kabakcı E, Köksal G. Ortoreksiya Nervoza ve ORTO-11’in Türkçeye Uyarlama Çalışması. Türk Psikiyatr Derg. 2008;19:283–291.
Cox JL, Holden JM, Sagovsky R. Detection of postnatal depression: development of the 10-item edinburgh postnatal depression scale. Br J Psychiatry. 1987;150:782–786.
Karaçam Z, Kiriş Y. The Postpartum Depression Screening Scale: its reliability and validity for the Turkish population. Turk Psikiyatr Derg. 2008;19:187–196.
Easter A, Solmi F, Bye A, Taborelli E, Corfield F, Schmidt U, et al. Antenatal and postnatal psychopathology among women with current and past eating disorders: longitudinal patterns. Eur Eat Disord Rev. 2015;23:19–27.
Angélica Nunes M, Poyastro Pinheiro A, Feliciati Hoffmann J, Inês Schmidt M. Eating disorders symptoms in pregnancy and postpartum: a prospective study in a disadvantaged population in Brazil. Int J Eat Disord. 2014;47:426–430.
Cici Saraç N, Bülbül S. Doğum sonrası kadınlarda beslenme bozukluklarının varlığının saptaması. Kırıkkale University; 2018. Master Thesis, Kırıkkale, Turkey.
Tayhan Kartal F, Yabancı Ayhan N. Relationship between eating disorders and internet and smartphone addiction in college students. Eat Weight Disord. 2020;26:1853–1862.
Kadioglu M, Ergun A. The eating attitudes of the university students, self-efficacy and affecting factors. J Marmara Univ Inst Heal Sci. 2015;5:96–104.
CDC. Increase the proportion of women delivering a live birth who had a healthy weight prior to pregnancy (Maternal Infant and Child Health). 2011. Available from: https://www.cdc.gov/nchs/data/hpdata2020/hp2020_FP_MICH_Progress_Review_Appendix.pdf
Linardon J, Braithwaite R, Cousins R, Brennan L. Appearance-based rejection sensitivity as a mediator of the relationship between symptoms of social anxiety and disordered eating cognitions and behaviors. Eat Behav. 2017;27:27–32.
Siega-Riz AM, Von Holle A, Haugen M, Meltzer HM, Hamer R, Torgersen L, et al. Gestational weight gain of women with eating disorders in the Norwegian pregnancy cohort. Int J Eat Disord. 2011;44:428–434.
Zerwas SC, Von Holle A, Perrin EM, Cockrell Skinner A, Reba-Harrelson L, Hamer RM, et al. Gestational and postpartum weight change patterns in mothers with eating disorders. Eur Eat Disord Rev. 2014;22:397–404.
Bergmeier H, Hill B, Haycraft E, Blewitt C, Lim S, Meyer C, et al. Maternal body dissatisfaction in pregnancy, postpartum and early parenting: An overlooked factor implicated in maternal and childhood obesity risk. Appetite. 2020;147:104525.
Koven N, Abry A. The clinical basis of orthorexia nervosa: emerging perspectives. Neuropsychiatr Dis Treat. 2015;18:385–394.
Altıner R, Okumuş F. Gebelerde Ortoreksiya Nervoza Eğiliminin Belirlenmesi. İstanbul Medipol University; 2019. Master Thesis, İstanbul, Turkey.
Ayhan Baser D, Cankurtaran M. The assessment of the orthorexia nervosa tendencies among postpartum women. Konuralp Med J 2021;13:218–225.
Arslantaş H. Eating behaviour and orthorexia nervosa (healthy eating obsession) in nursing students: cross-sectional analytic study. J Psychiatr Nurs. 2017;8:137–143.
Gezer C, Kabaran S. Orthorexia nervosa: is it a risk for female students studying nutrition and dietetics? Süleyman Demirel Üniversitesi Sağlık Bilim Derg. 2013;4:14–22.
Arusoğlu G. Healthy eating obsession (orthorexia): examination of the symptoms, the adaptation of ORTO-15. [In Turkish.] Ankara, Turkey: Hacettepe University; 2006.
Franko DL, Walton BE. Pregnancy and eating disorders: a review and clinical implications. Int J Eat Disord. 1993;13:41–47.
Lovering ME, Rodgers RF, George JE, Franko DL. Exploring the tripartite influence model of body dissatisfaction in postpartum women. Body Image. 2018;24:44–54.
Shorey S, Chee CYI, Ng ED, Chan YH, Tam WWS, Chong YS. Prevalence and incidence of postpartum depression among healthy mothers: a systematic review and meta-analysis. J Psychiatr Res. 2018;104:235–248.
Moroze RM, Dunn TM, Craig Holland J, Yager J, Weintraub P. Microthinking about micronutrients: a case of transition from obsessions about healthy eating to near-fatal “orthorexia nervosa” and proposed diagnostic criteria. Psychosomatics. 2015;56:397–403.
Lopes R, Melo R, Dias Pereira B. Orthorexia nervosa and comorbid depression successfully treated with mirtazapine: a case report. Eat Weight Disord. 2020;25:163–167.
Luck-Sikorski C, Jung F, Schlosser K, Riedel-Heller SG. Is orthorexic behavior common in the general public? A large representative study in Germany. Eat Weight Disord. 2019;24:267–273.
Author information
Authors and Affiliations
Contributions
FT was responsible for conceptualizing the research protocol, writing the protocol and report, conducting the research, analyzing data, interpreting results, adjusting the manuscript according to the comments of co-authors, updating reference lists and forming ‘Summary of findings’ tables. GD and NYA were responsible for designing the research protocol and screening potentially appropriate studies. They provided a review and critical evaluation of the manuscript. CS contributed to collecting the data.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Tayhan, F., Doğan, G., Yabancı Ayhan, N. et al. Assessment of eating disorders and depression in postpartum women. Eur J Clin Nutr 78, 314–319 (2024). https://doi.org/10.1038/s41430-023-01384-7
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41430-023-01384-7