Abstract
Malaria, mostly due to Plasmodium falciparum infection in Africa, remains one of the most important infectious diseases in the world. Standard treatment for uncomplicated P. falciparum malaria is artemisinin-based combination therapy (ACT), which includes a rapid-acting artemisinin derivative plus a longer-acting partner drug, and standard therapy for severe P. falciparum malaria is intravenous artesunate. The efficacy of artemisinins and ACT has been threatened by the emergence of artemisinin partial resistance in Southeast Asia, mediated principally by mutations in the P. falciparum Kelch 13 (K13) protein. High ACT treatment failure rates have occurred when resistance to partner drugs is also seen. Recently, artemisinin partial resistance has emerged in Rwanda, Uganda and the Horn of Africa, with independent emergences of different K13 mutants in each region. In this Review, we summarize our current knowledge of artemisinin partial resistance and focus on the emergence of resistance in Africa, including its epidemiology, transmission dynamics and mechanisms. At present, the clinical impact of emerging resistance in Africa is unclear and most available evidence suggests that the efficacies of leading ACTs remain excellent, but there is an urgent need to better appreciate the extent of the problem and its consequences for the treatment and control of malaria.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$29.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
Change history
27 February 2024
A Correction to this paper has been published: https://doi.org/10.1038/s41579-024-01032-2
References
World Health Organization. World Malaria Report (WHO, 2022).
Haldar, K., Bhattacharjee, S. & Safeukui, I. Drug resistance in Plasmodium. Nat. Rev. Microbiol. 16, 156–170 (2018).
Plowe, C. V. Malaria chemoprevention and drug resistance: a review of the literature and policy implications. Malar. J. 21, 104 (2022).
Ward, K. E., Fidock, D. A. & Bridgford, J. L. Plasmodium falciparum resistance to artemisinin-based combination therapies. Curr. Opin. Microbiol. 69, 102193 (2022).
World Health Organization. WHO Guidelines for Malaria (WHO, 2022).
Noedl, H., Se, Y., Schaecher, K., Smith, B. L., Socheat, D. & Fukuda, M. M. Evidence of artemisinin-resistant malaria in western Cambodia. N. Engl. J. Med. 359, 2619–2620 (2008).
Dondorp, A. M. et al. Artemisinin resistance in Plasmodium falciparum malaria. N. Engl. J. Med. 361, 455–467 (2009).
Conrad, M. D. & Rosenthal, P. J. Antimalarial drug resistance in Africa: the calm before the storm? Lancet Infect. Dis. 19, e338–e351 (2019).
Tu, Y. The discovery of artemisinin (qinghaosu) and gifts from Chinese medicine. Nat. Med. 17, 1217–1220 (2011).
Klayman, D. L. Qinghaosu (artemisinin): an antimalarial drug from China. Science 228, 1049–1055 (1985).
White, N. J. Qinghaosu (artemisinin): the price of success. Science 320, 330–334 (2008).
Miller, L. H. & Su, X. Artemisinin: discovery from the Chinese herbal garden. Cell 146, 855–858 (2011).
Ma, N., Zhang, Z., Liao, F., Jiang, T. & Tu, Y. The birth of artemisinin. Pharmacol. Ther. 216, 107658 (2020).
Jiang, J. B., Li, G. Q., Guo, X. B., Kong, Y. C. & Arnold, K. Antimalarial activity of mefloquine and qinghaosu. Lancet 2, 285–288 (1982).
Li, G. Q., Arnold, K., Guo, X. B., Jian, H. X. & Fu, L. C. Randomised comparative study of mefloquine, qinghaosu, and pyrimethamine-sulfadoxine in patients with falciparum malaria. Lancet 2, 1360–1361 (1984).
Nosten, F. & White, N. J. Artemisinin-based combination treatment of falciparum malaria. Am. J. Trop. Med. Hyg. 77, 181–192 (2007).
Nosten, F. et al. Treatment of multidrug-resistant Plasmodium falciparum malaria with 3-day artesunate-mefloquine combination. J. Infect. Dis. 170, 971–977 (1994).
Nosten, F. et al. Effects of artesunate-mefloquine combination on incidence of Plasmodium falciparum malaria and mefloquine resistance in western Thailand: a prospective study. Lancet 356, 297–302 (2000).
Price, R. N. et al. Mefloquine resistance in Plasmodium falciparum and increased pfmdr1 gene copy number. Lancet 364, 438–447 (2004).
Vugt, M. V. et al. Efficacy of six doses of artemether-lumefantrine (benflumetol) in multidrug-resistant Plasmodium falciparum malaria. Am. J. Trop. Med. Hyg. 60, 936–942 (1999).
West African Network for Clinical Trials of Antimalarial Drugs (WANECAM). Pyronaridine-artesunate or dihydroartemisinin-piperaquine versus current first-line therapies for repeated treatment of uncomplicated malaria: a randomised, multicentre, open-label, longitudinal, controlled, phase 3b/4 trial. Lancet 391, 1378–1390 (2018).
Dondorp, A., Nosten, F., Stepniewska, K., Day, N. & White, N. Artesunate versus quinine for treatment of severe falciparum malaria: a randomised trial. Lancet 366, 717–725 (2005).
Dondorp, A. M. et al. Artesunate versus quinine in the treatment of severe falciparum malaria in African children (AQUAMAT): an open-label, randomised trial. Lancet 376, 1647–1657 (2010).
Meshnick, S. R. Artemisinin: mechanisms of action, resistance and toxicity. Int. J. Parasitol. 32, 1655–1660 (2002).
Rosenthal, P. J. & Meshnick, S. R. Hemoglobin catabolism and iron utilization by malaria parasites. Mol. Biochem. Parasitol. 83, 131–139 (1996).
Sigala, P. A. & Goldberg, D. E. The peculiarities and paradoxes of Plasmodium heme metabolism. Annu. Rev. Microbiol. 68, 259–278 (2014).
Heller, L. E. & Roepe, P. D. Artemisinin-based antimalarial drug therapy: molecular pharmacology and evolving resistance. Trop. Med. Infect. Dis. 4, 89 (2019).
Klonis, N. et al. Artemisinin activity against Plasmodium falciparum requires hemoglobin uptake and digestion. Proc. Natl Acad. Sci. USA 108, 11405–11410 (2011).
Wang, J. et al. Haem-activated promiscuous targeting of artemisinin in Plasmodium falciparum. Nat. Commun. 6, 10111 (2015).
Bridgford, J. L. et al. Artemisinin kills malaria parasites by damaging proteins and inhibiting the proteasome. Nat. Commun. 9, 3801 (2018).
Dhorda, M., Amaratunga, C. & Dondorp, A. M. Artemisinin and multidrug-resistant Plasmodium falciparum — a threat for malaria control and elimination. Curr. Opin. Infect. Dis. 34, 432–439 (2021).
Witkowski, B. et al. Novel phenotypic assays for the detection of artemisinin-resistant Plasmodium falciparum malaria in Cambodia: in-vitro and ex-vivo drug-response studies. Lancet Infect. Dis. 13, 1043–1049 (2013).
Ariey, F. et al. A molecular marker of artemisinin-resistant Plasmodium falciparum malaria. Nature 505, 50–55 (2014).
Straimer, J. et al. Drug resistance. K13-propeller mutations confer artemisinin resistance in Plasmodium falciparum clinical isolates. Science 347, 428–431 (2015).
WWARN K13 Genotype-Phenotype Study Group. Association of mutations in the Plasmodium falciparum Kelch13 gene (Pf3D7_1343700) with parasite clearance rates after artemisinin-based treatments-a WWARN individual patient data meta-analysis. BMC Med. 17, 1 (2019).
Miotto, O. et al. Genetic architecture of artemisinin-resistant Plasmodium falciparum. Nat. Genet. 47, 226–234 (2015).
Paloque, L. et al. Mutation in the Plasmodium falciparum BTB/POZ domain of K13 protein confers artemisinin resistance. Antimicrob. Agents Chemother. 66, e0132021 (2022).
Barrett, M. P., Kyle, D. E., Sibley, L. D., Radke, J. B. & Tarleton, R. L. Protozoan persister-like cells and drug treatment failure. Nat. Rev. Microbiol. 17, 607–620 (2019).
Sutherland, C. J., Henrici, R. C. & Artavanis-Tsakonas, K. Artemisinin susceptibility in the malaria parasite Plasmodium falciparum: propellers, adaptor proteins and the need for cellular healing. FEMS Microbiol. Rev. 45, fuaa056 (2021).
Siddiqui, F. A., Liang, X. & Cui, L. Plasmodium falciparum resistance to ACTs: emergence, mechanisms, and outlook. Int. J. Parasitol. Drugs Drug Resist. 16, 102–118 (2021).
Mok, S. et al. Drug resistance. Population transcriptomics of human malaria parasites reveals the mechanism of artemisinin resistance. Science 347, 431–435 (2015).
Mok, S. et al. Artemisinin-resistant K13 mutations rewire Plasmodium falciparum’s intra-erythrocytic metabolic program to enhance survival. Nat. Commun. 12, 530 (2021).
Zhu, L. et al. Artemisinin resistance in the malaria parasite, Plasmodium falciparum, originates from its initial transcriptional response. Commun. Biol. 5, 274 (2022).
Xiong, A. et al. K13-mediated reduced susceptibility to artemisinin in Plasmodium falciparum Is overlaid on a trait of enhanced DNA damage repair. Cell Rep. 32, 107996 (2020).
Connelly, S. V. et al. Restructured mitochondrial-nuclear interaction in Plasmodium falciparum dormancy and persister survival after artemisinin exposure. mBio 12, e0075321 (2021).
Mbengue, A. et al. A molecular mechanism of artemisinin resistance in Plasmodium falciparum malaria. Nature 520, 683–687 (2015).
Birnbaum, J. et al. A Kelch13-defined endocytosis pathway mediates artemisinin resistance in malaria parasites. Science 367, 51–59 (2020).
Siddiqui, G., Srivastava, A., Russell, A. S. & Creek, D. J. Multi-omics based identification of specific biochemical changes associated with PfKelch13-mutant artemisinin-resistant Plasmodium falciparum. J. Infect. Dis. 215, 1435–1444 (2017).
Yang, T. et al. Decreased K13 abundance reduces hemoglobin catabolism and proteotoxic stress, underpinning artemisinin resistance. Cell Rep. 29, 2917–2928.e5 (2019).
Gnadig, N. F. et al. Insights into the intracellular localization, protein associations and artemisinin resistance properties of Plasmodium falciparum K13. PLoS Pathog. 16, e1008482 (2020).
Xie, S. C. et al. Haemoglobin degradation underpins the sensitivity of early ring stage Plasmodium falciparum to artemisinins. J. Cell Sci. 129, 406–416 (2016).
Stokes, B. H. et al. Plasmodium falciparum K13 mutations in Africa and Asia impact artemisinin resistance and parasite fitness. eLife 10, e66277 (2021).
Xie, S. C., Ralph, S. A. & Tilley, L. K13, the cytostome, and artemisinin resistance. Trends Parasitol. 36, 533–544 (2020).
Hunt, P. et al. Gene encoding a deubiquitinating enzyme is mutated in artesunate- and chloroquine-resistant rodent malaria parasites. Mol. Microbiol. 65, 27–40 (2007).
Simwela, N. V., Hughes, K. R., Roberts, A. B., Rennie, M. T., Barrett, M. P. & Waters, A. P. Experimentally engineered mutations in a ubiquitin hydrolase, UBP-1, modulate in vivo susceptibility to artemisinin and chloroquine in Plasmodium berghei. Antimicrob. Agents Chemother. 64, e02484-19 (2020).
Henrici, R. C., van Schalkwyk, D. A. & Sutherland, C. J. Modification of pfap2mu and pfubp1 markedly reduces ring-stage susceptibility of Plasmodium falciparum to artemisinin in vitro. Antimicrob. Agents Chemother. 64, e01542-19 (2019).
Henriques, G. et al. Directional selection at the pfmdr1, pfcrt, pfubp1, and pfap2mu loci of Plasmodium falciparum in Kenyan children treated with ACT. J. Infect. Dis. 210, 2001–2008 (2014).
Tumwebaze, P. K. et al. Decreased susceptibility of Plasmodium falciparum to both dihydroartemisinin and lumefantrine in northern Uganda. Nat. Commun. 13, 6353 (2022).
Henriques, G. et al. The Mu subunit of Plasmodium falciparum clathrin-associated adaptor protein 2 modulates in vitro parasite response to artemisinin and quinine. Antimicrob. Agents Chemother. 59, 2540–2547 (2015).
Olshina, M. A. et al. Plasmodium falciparum coronin organizes arrays of parallel actin filaments potentially guiding directional motility in invasive malaria parasites. Malar. J. 14, 280 (2015).
Demas, A. R. et al. Mutations in Plasmodium falciparum actin-binding protein coronin confer reduced artemisinin susceptibility. Proc. Natl Acad. Sci. USA 115, 12799–12804 (2018).
Rosenthal, P. J. Falcipain cysteine proteases of malaria parasites: an update. Biochim. Biophys. Acta Proteins Proteom. 1868, 140362 (2020).
Siddiqui, F. A. et al. Plasmodium falciparum falcipain-2a polymorphisms in Southeast Asia and their association with artemisinin resistance. J. Infect. Dis. 218, 434–442 (2018).
Wang, J., Xu, C., Lun, Z. R. & Meshnick, S. R. Unpacking ‘artemisinin resistance’. Trends Pharmacol. Sci. 38, 506–511 (2017).
Ashley, E. A. et al. Spread of artemisinin resistance in Plasmodium falciparum malaria. N. Engl. J. Med. 371, 411–423 (2014).
Phyo, A. P. et al. Declining efficacy of artemisinin combination therapy against P. falciparum malaria on the Thai-Myanmar border (2003-2013): the role of parasite genetic factors. Clin. Infect. Dis. 63, 784–791 (2016).
Amaratunga, C. et al. Dihydroartemisinin-piperaquine resistance in Plasmodium falciparum malaria in Cambodia: a multisite prospective cohort study. Lancet Infect. Dis. 16, 357–365 (2016).
Mairet-Khedim, M. et al. Clinical and in vitro resistance of Plasmodium falciparum to artesunate-amodiaquine in Cambodia. Clin. Infect. Dis. 73, 406–413 (2021).
Kagoro, F. M. et al. Mapping genetic markers of artemisinin resistance in Plasmodium falciparum malaria in Asia: a systematic review and spatiotemporal analysis. Lancet Microbe 3, e184–e192 (2022).
Takala-Harrison, S. et al. Independent emergence of artemisinin resistance mutations among Plasmodium falciparum in Southeast Asia. J. Infect. Dis. 211, 670–679 (2015).
Amato, R. et al. Origins of the current outbreak of multidrug-resistant malaria in southeast Asia: a retrospective genetic study. Lancet Infect. Dis. 18, 337–345 (2018).
Hamilton, W. L. et al. Evolution and expansion of multidrug-resistant malaria in southeast Asia: a genomic epidemiology study. Lancet Infect. Dis. 19, 943–951 (2019).
Imwong, M. et al. Molecular epidemiology of resistance to antimalarial drugs in the Greater Mekong subregion: an observational study. Lancet Infect. Dis. 20, 1470–1480 (2020).
Wasakul, V. et al. Malaria outbreak in Laos driven by a selective sweep for Plasmodium falciparum kelch13 R539T mutants: a genetic epidemiology analysis. Lancet Infect. Dis. 23, 568–577 (2023).
Chenet, S. M. et al. Independent emergence of the Plasmodium falciparum kelch Propeller domain mutant allele C580Y in Guyana. J. Infect. Dis. 213, 1472–1475 (2016).
Mathieu, L. C. et al. Local emergence in Amazonia of Plasmodium falciparum k13 C580Y mutants associated with in vitro artemisinin resistance. eLife 9, e51015 (2020).
Miotto, O. et al. Emergence of artemisinin-resistant Plasmodium falciparum with kelch13 C580Y mutations on the island of New Guinea. PLoS Pathog. 16, e1009133 (2020).
Yoshida, N., Yamauchi, M., Morikawa, R., Hombhanje, F. & Mita, T. Increase in the proportion of Plasmodium falciparum with kelch13 C580Y mutation and decline in pfcrt and pfmdr1 mutant alleles in Papua New Guinea. Malar. J. 20, 410 (2021).
Lautu-Gumal, D. et al. Surveillance of molecular markers of Plasmodium falciparum artemisinin resistance (kelch13 mutations) in Papua New Guinea between 2016 and 2018. Int. J. Parasitol. Drugs Drug Resist. 16, 188–193 (2021).
Das, S., Saha, B., Hati, A. K. & Roy, S. Evidence of artemisinin-resistant Plasmodium falciparum malaria in eastern India. N. Engl. J. Med. 379, 1962–1964 (2018).
Das, S., Manna, S., Saha, B., Hati, A. K. & Roy, S. Novel pfkelch13 gene polymorphism associates With artemisinin resistance in eastern India. Clin. Infect. Dis. 69, 1144–1152 (2019).
Rana, R. et al. Sequence analysis of the K13-propeller gene in artemisinin challenging Plasmodium falciparum isolates from malaria endemic areas of Odisha, India: a molecular surveillance study. Biomed. Res. Int. 2020, 8475246 (2020).
Wedam, J. et al. Molecular evidence for Plasmodium falciparum resistance to sulfadoxine-pyrimethamine but absence of K13 mutations in Mangaluru, southwestern India. Am. J. Trop. Med. Hyg. 99, 1508–1510 (2018).
Menard, D. et al. A worldwide map of Plasmodium falciparum K13-propeller polymorphisms. N. Engl. J. Med. 374, 2453–2464 (2016).
Taylor, S. M. et al. Absence of putative artemisinin resistance mutations among Plasmodium falciparum in sub-Saharan Africa: a molecular epidemiologic study. J. Infect. Dis. 211, 680–688 (2015).
Kamau, E. et al. K13-propeller polymorphisms in Plasmodium falciparum parasites from sub-Saharan Africa. J. Infect. Dis. 211, 1352–1355 (2015).
Conrad, M. D. et al. Polymorphisms in K13 and falcipain-2 associated with artemisinin resistance are not prevalent in Plasmodium falciparum isolated from Ugandan children. PLoS ONE 9, e105690 (2014).
Cooper, R. A. et al. Lack of artemisinin resistance in Plasmodium falciparum in Uganda based on parasitological and molecular assays. Antimicrob. Agents Chemother. 59, 5061–5064 (2015).
Ndwiga, L. et al. A review of the frequencies of Plasmodium falciparum Kelch 13 artemisinin resistance mutations in Africa. Int. J. Parasitol. Drugs Drug Resist. 16, 155–161 (2021).
Tacoli, C. et al. Artemisinin resistance-associated K13 polymorphisms of Plasmodium falciparum in southern Rwanda, 2010-2015. Am. J. Trop. Med. Hyg. 95, 1090–1093 (2016).
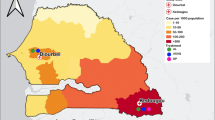
Kirby, R. et al. Examining the early distribution of the artemisinin-resistant Plasmodium falciparum kelch13 R561H mutation in areas of higher transmission in Rwanda. Open Forum Infect. Dis. 10, ofad149 (2023).
Uwimana, A. et al. Emergence and clonal expansion of in vitro artemisinin-resistant Plasmodium falciparum kelch13 R561H mutant parasites in Rwanda. Nat. Med. 26, 1602–1608 (2020).
Uwimana, A. et al. Association of Plasmodium falciparum kelch13 R561H genotypes with delayed parasite clearance in Rwanda: an open-label, single-arm, multicentre, therapeutic efficacy study. Lancet Infect. Dis. 21, 1120–1128 (2021).
Straimer, J., Gandhi, P., Renner, K. C. & Schmitt, E. K. High prevalence of Plasmodium falciparum K13 mutations in Rwanda is associated with slow parasite clearance after treatment with artemether-lumefantrine. J. Infect. Dis. 225, 1411–1414 (2022).
Bergmann, C. et al. Increase in Kelch 13 polymorphisms in Plasmodium falciparum, southern Rwanda. Emerg. Infect. Dis. 27, 294–296 (2021).
Moser, K. A. et al. Describing the current status of Plasmodium falciparum population structure and drug resistance within mainland Tanzania using molecular inversion probes. Mol. Ecol. 30, 100–113 (2021).
Bwire, G. M., Ngasala, B., Mikomangwa, W. P., Kilonzi, M. & Kamuhabwa, A. A. R. Detection of mutations associated with artemisinin resistance at k13-propeller gene and a near complete return of chloroquine susceptible falciparum malaria in Southeast of Tanzania. Sci. Rep. 10, 3500 (2020).
Juliano, J. J. et al. Country wide surveillance reveals prevalent artemisinin partial resistance mutations with evidence for multiple origins and expansion of high level sulfadoxine-pyrimethamine resistance mutations in northwest Tanzania. Preprint at: medRxiv https://doi.org/10.1101/2023.11.07.23298207 (2023).
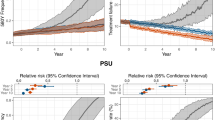
Conrad, M. D. et al. Evolution of partial resistance to artemisinins in malaria parasites in Uganda. N. Engl. J. Med. 389, 722–732 (2023).
Mihreteab, S. et al. Increasing prevalence of artemisinin-resistant HRP2-negative malaria in Eritrea. N. Engl. J. Med. 389, 1191–1202 (2023).
Tumwebaze, P. et al. Changing antimalarial drug resistance patterns identified by surveillance at three sites in Uganda. J. Infect. Dis. 215, 631–635 (2017).
Rasmussen, S. A. et al. Changing antimalarial drug sensitivities in Uganda. Antimicrob. Agents Chemother. 61, e01516-17 (2017).
Conrad, M. D., Nsobya, S. L. & Rosenthal, P. J. The diversity of the Plasmodium falciparum K13 propeller domain did not increase after implementation of artemisinin-based combination therapy in Uganda. Antimicrob. Agents Chemother. 63, e01234-19 (2019).
Ikeda, M. et al. Artemisinin-resistant Plasmodium falciparum with high survival rates, Uganda, 2014-2016. Emerg. Infect. Dis. 24, 718–726 (2018).
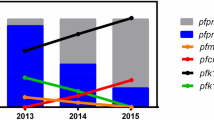
Asua, V. et al. Changing molecular markers of antimalarial drug sensitivity across Uganda. Antimicrob. Agents Chemother. 63, e01818-18 (2019).
Asua, V. et al. Changing prevalence of potential mediators of aminoquinoline, antifolate, and artemisinin resistance across Uganda. J. Infect. Dis. 223, 985–994 (2021).
Balikagala, B. et al. Evidence of artemisinin-resistant malaria in Africa. N. Engl. J. Med. 385, 1163–1171 (2021).
Pacheco, M. A. et al. Evolution and genetic diversity of the k13 gene associated with artemisinin delayed parasite clearance in Plasmodium falciparum. Antimicrob. Agents Chemother. 63, e02550-18 (2019).
Matrevi, S. A. et al. Plasmodium falciparum kelch propeller polymorphisms in clinical isolates from Ghana from 2007 to 2016. Antimicrob. Agents Chemother. 63, e00802-19 (2019).
Mensah, B. A. et al. Antimalarial drug resistance profiling of Plasmodium falciparum infections in Ghana using molecular inversion probes and next-generation sequencing. Antimicrob. Agents Chemother. 64, e01423-19 (2020).
Bayih, A. G., Getnet, G., Alemu, A., Getie, S., Mohon, A. N. & Pillai, D. R. A unique Plasmodium falciparum K13 gene mutation in northwest Ethiopia. Am. J. Trop. Med. Hyg. 94, 132–135 (2016).
Alemayehu, A. A. et al. Expansion of the Plasmodium falciparum Kelch 13 R622I mutation in Northwest Ethiopia. Preprint at: Res. Sq. https://doi.org/10.21203/rs.3.rs-171038/v1 (2021).
Emiru, T. et al. Evidence for a role of Anopheles stephensi in the spread of drug and diagnosis-resistant malaria in Africa. Nat. Med. 29, 3203–3211 (2023).
Fola, A. A. et al. Plasmodium falciparum resistant to artemisinin and diagnostics have emerged in Ethiopia. Nat. Microbiol. 8, 1911–1919 (2023).
Owoloye, A., Olufemi, M., Idowu, E. T. & Oyebola, K. M. Prevalence of potential mediators of artemisinin resistance in African isolates of Plasmodium falciparum. Malar. J. 20, 451 (2021).
van Loon, W. et al. In vitro confirmation of artemisinin resistance in Plasmodium falciparum from patient isolates, Southern Rwanda, 2019. Emerg. Infect. Dis. 28, 852–855 (2022).
Straimer, J., Gnadig, N. F., Stokes, B. H., Ehrenberger, M., Crane, A. A. & Fidock, D. A. Plasmodium falciparum K13 mutations differentially impact ozonide susceptibility and parasite fitness in vitro. mBio 8, e00172-17 (2017).
Nair, S. et al. Fitness costs and the rapid spread of kelch13-C580Y substitutions conferring artemisinin resistance. Antimicrob. Agents Chemother. 62, e00605-18 (2018).
Stokes, B. H., Ward, K. E. & Fidock, D. A. Evidence of artemisinin-resistant malaria in Africa. N. Engl. J. Med. 386, 1385–1386 (2022).
Wang, L. T. et al. Private sector drug shops frequently dispense parenteral anti-malarials in a rural region of Western Uganda. Malar. J. 17, 305 (2018).
Blasco, B., Leroy, D. & Fidock, D. A. Antimalarial drug resistance: linking Plasmodium falciparum parasite biology to the clinic. Nat. Med. 23, 917–928 (2017).
Sidhu, A. B., Uhlemann, A. C., Valderramos, S. G., Valderramos, J. C., Krishna, S. & Fidock, D. A. Decreasing pfmdr1 copy number in Plasmodium falciparum malaria heightens susceptibility to mefloquine, lumefantrine, halofantrine, quinine, and artemisinin. J. Infect. Dis. 194, 528–535 (2006).
Tumwebaze, P. K. et al. Drug susceptibility of Plasmodium falciparum in eastern Uganda: a longitudinal phenotypic and genotypic study. Lancet Microbe 2, e441–e449 (2021).
Phuc, B. Q. et al. Treatment failure of dihydroartemisinin/piperaquine for Plasmodium falciparum malaria, Vietnam. Emerg. Infect. Dis. 23, 715–717 (2017).
van der Pluijm, R. W. et al. Determinants of dihydroartemisinin-piperaquine treatment failure in Plasmodium falciparum malaria in Cambodia, Thailand, and Vietnam: a prospective clinical, pharmacological, and genetic study. Lancet Infect. Dis. 19, 952–961 (2019).
Wicht, K. J., Small-Saunders, J. L., Hagenah, L. M., Mok, S. & Fidock, D. A. Mutant PfCRT can mediate piperaquine resistance in African Plasmodium falciparum with reduced fitness and increased susceptibility to other antimalarials. J. Infect. Dis. 226, 2021–2029 (2022).
Florimond, C. et al. Impact of piperaquine resistance in Plasmodium falciparum on malaria treatment effectiveness in French Guiana: a descriptive epidemiological study.Lancet Infect. Dis. https://doi.org/10.1016/S1473-3099(23)00502-9 (2023).
Leang, R. et al. Efficacy and safety of pyronaridine-artesunate for treatment of uncomplicated Plasmodium falciparum malaria in western Cambodia. Antimicrob. Agents Chemother. 60, 3884–3890 (2016).
Leang, R. et al. Efficacy and safety of pyronaridine-artesunate plus single-dose primaquine for treatment of uncomplicated Plasmodium falciparum malaria in eastern Cambodia. Antimicrob. Agents Chemother. 63, e02242-18 (2019).
Quang Bui, P. et al. Pyronaridine-artesunate efficacy and safety in uncomplicated Plasmodium falciparum malaria in areas of artemisinin-resistant falciparum in Viet Nam (2017-2018). Clin. Infect. Dis. 70, 2187–2195 (2020).
Leang, R. et al. Efficacy and safety of pyronaridine-artesunate plus single-dose primaquine for the treatment of malaria in western Cambodia. Antimicrob. Agents Chemother. 63, e01273-19 (2019).
Rahi, M., Chaturvedi, R., Goswami, R. & Sharma, A. India needs to consider planning a change to artemether-lumefantrine to treat Plasmodium falciparum malaria. Am. J. Trop. Med. Hyg. 106, 1305–1310 (2022).
Dimbu, P. R. et al. Continued low efficacy of artemether-lumefantrine in Angola in 2019. Antimicrob. Agents Chemother. 65, e01949-20 (2021).
Moriarty, L. F. et al. Therapeutic efficacy of artemisinin-based combination therapies in Democratic Republic of the Congo and investigation of molecular markers of antimalarial resistance. Am. J. Trop. Med. Hyg. 105, 1067–1075 (2021).
Gansane, A. et al. Anti-malarial efficacy and resistance monitoring of artemether-lumefantrine and dihydroartemisinin-piperaquine shows inadequate efficacy in children in Burkina Faso, 2017-2018. Malar. J. 20, 48 (2021).
Ebong, C. et al. Efficacy and safety of artemether-lumefantrine and dihydroartemisinin-piperaquine for the treatment of uncomplicated Plasmodium falciparum malaria and prevalence of molecular markers associated with artemisinin and partner drug resistance in Uganda. Malar. J. 20, 484 (2021).
Rasmussen, C. & Ringwald, P. Continued low efficacy of artemether-lumefantrine in Angola? Antimicrob. Agents Chemother. 65, e00220-21 (2021).
Rasmussen, C. & Ringwald, P. Is there evidence of anti-malarial multidrug resistance in Burkina Faso? Malar. J. 20, 320 (2021).
Hastings, I. M. & Felger, I. WHO antimalarial trial guidelines: good science, bad news? Trends Parasitol. 38, 933–941 (2022).
Plucinski, M. M., Hastings, I. M., Moriarty, L. F., Venkatesan, M., Felger, I. & Halsey, E. S. Variation in calculating and reporting antimalarial efficacy against Plasmodium falciparum in sub-Saharan Africa: a systematic review of published reports. Am. J. Trop. Med. Hyg. 104, 1820–1829 (2021).
Wakoli, D. M. et al. Impact of parasite genomic dynamics on the sensitivity of Plasmodium falciparum isolates to piperaquine and other antimalarial drugs. BMC Med. 20, 448 (2022).
Ofori, M. F. et al. Ex vivo sensitivity Profile of Plasmodium falciparum clinical isolates to a panel of antimalarial drugs in Ghana 13 years after national policy change. Infect. Drug. Resist. 14, 267–276 (2021).
Traore, K. et al. Ex-vivo sensitivity of Plasmodium falciparum to common anti-malarial drugs: the case of Kenieroba, a malaria endemic village in Mali. Drugs R. D. 20, 249–255 (2020).
van der Pluijm, R. W. et al. Triple artemisinin-based combination therapies versus artemisinin-based combination therapies for uncomplicated Plasmodium falciparum malaria: a multicentre, open-label, randomised clinical trial. Lancet 395, 1345–1360 (2020).
Acknowledgements
Work by the authors is supported by the National Institutes of Health (R01AI075045, R01AI117001, R01AI139179, U01AI141308, U19AI089674 to P.J.R.; R01AI173557 to M.D.C.); The Bill and Melinda Gates Foundation (INV-035751); and the Medicines for Malaria Venture. V.A. is the recipient of a PAMAfrica PhD fellowship, supported by the European & Developing Countries Clinical Trials Partnership. The authors thank David Fidock, Columbia University, for a critical review of this manuscript, and Faiza Siddiqui and Liwang Cui, University of South Florida, for generously providing Fig. 4.
Author information
Authors and Affiliations
Contributions
All authors reviewed the literature, synthesized available data, and contributed to the writing of this manuscript.
Corresponding author
Ethics declarations
Competing interests
There are no competing interests.
Peer review
Peer review information
Nature Reviews Microbiology thanks Didier Ménard, Lorenz Von Seidlein and the other, anonymous, reviewer(s) for their contribution to the peer review of this work.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Related links
Malaria: Artemisinin partial resistance: https://www.who.int/news-room/questions-and-answers/item/artemisinin-resistance
Rights and permissions
Springer Nature or its licensor (e.g. a society or other partner) holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Rosenthal, P.J., Asua, V. & Conrad, M.D. Emergence, transmission dynamics and mechanisms of artemisinin partial resistance in malaria parasites in Africa. Nat Rev Microbiol 22, 373–384 (2024). https://doi.org/10.1038/s41579-024-01008-2
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41579-024-01008-2
This article is cited by
-
Expansion of artemisinin partial resistance mutations and lack of histidine rich protein-2 and -3 deletions in Plasmodium falciparum infections from Rukara, Rwanda
Malaria Journal (2024)
-
tRNA modification reprogramming contributes to artemisinin resistance in Plasmodium falciparum
Nature Microbiology (2024)
-
Urgent action is needed to confront artemisinin partial resistance in African malaria parasites
Nature Medicine (2024)