Abstract
This cross-sectional study, conducted between January 2020 and July 2023, aimed to assess the knowledge, attitude, and post-traumatic stress symptoms (PTSS) among parents with children undergoing extracorporeal membrane oxygenation (ECMO) treatment. Out of 201 valid questionnaires collected, the median knowledge score was 3.00, the mean attitude score was 27.00 ± 3.20, and the mean PTSS score was 3.50 ± 1.54. Logistic regression identified associations between PTSS and parents with lower education levels, particularly junior high school and high school/technical secondary school education, as well as those occupied as housewives. Structural equation modeling highlighted direct effects, such as the impact of residence on education, education on employment status, and associations between knowledge, attitude, PTSS, employment status, monthly income, and parental demographics. The findings indicated inadequate knowledge and suboptimal attitudes among parents, especially those with lower education levels, emphasizing the need for educational resources. Furthermore, addressing parental PTSS through psychosocial support and screening was deemed essential, providing valuable insights for tailored interventions in this context.
Similar content being viewed by others
Introduction
Extracorporeal Membrane Oxygenation (ECMO) has seen significant growth in its applications for treating severe acute respiratory failure (Veno-Venous ECMO) and circulatory failure (Veno-Arterial ECMO)1. This expansion is largely attributed to advancements in ECMO technology and increased clinical experience2. The number of pediatric patients benefiting from ECMO support has also been on the rise, with the Extracorporeal Life Support Organization (ELSO) reporting 3249 infants and children receiving ECMO in 20153. Notably, neonatal and pediatric ECMO cases constitute nearly 50% and 25% of the total ECMO interventions, respectively, according to ELSO's registry data4. Symptoms of post-traumatic stress disorder (PTSD) emerge subsequent to the experience of a significantly distressing event. These symptoms collectively manifest as a syndrome characterized by heightened arousal and agitation, recurrent re-experiencing of the traumatic event, and deliberate avoidance of stimuli associated with the trauma5. Concurrently, it is essential to consider the psychological ramifications, as Post-traumatic stress symptoms (PTSS) can result from traumatic experiences, and a child's critical illness can be profoundly distressing for parents, potentially leading to symptoms of Acute Stress Disorder (ASD), PTSS, and full-fledged PTSS within the family unit, highlighting the critical need for comprehensive research and support in this context6,7.
A Knowledge, Attitude, and Practices (KAP) survey is a diagnostic research methodology used to assess a specific group's comprehension, viewpoints, and actions regarding a particular subject matter, encompassing their knowledge, attitudes, and behavioral patterns related to the designated topic8,9,10. Given the urgent and highly stressful nature of ECMO therapy, which can have lasting psychological effects on patient families, and the limited exploration of the psychological and emotional impact of ECMO in existing research, examining parents' knowledge and attitudes towards ECMO is important. This study may help medical teams better understand the needs of ECMO patient families, improve communication, provide appropriate support, and guide the development of interventions for their psychological well-being, while also offering insights for further research in related areas.
Healthcare providers should be aware of the elevated rates of post-traumatic stress experienced by parents of children who have survived critical illness11. Implementing routine screening for post-traumatic stress symptoms and offering support resources can facilitate early intervention. A longitudinal study12 found that family members primarily relied on problem-focused coping strategies, with anxiety symptoms peaking during treatment initiation but gradually decreasing over time, along with reductions in depression and PTSD symptoms. However, Health-Related Quality of Life (HRQOL) remained significantly impaired, indicating persistent emotional distress despite symptom improvement. Similarly, a retrospective analysis13 identified a high prevalence of PTSD symptoms among adult survivors of veno-arterial ECMO (VA-ECMO) support, particularly in patients with longer ICU stays requiring sedation and mechanical ventilation, underscoring the potential psychological impact of prolonged critical care treatment. Despite its significance, there has been a lack of KAP studies in this area. Therefore, this study aimed to investigate knowledge, attitude, and parental PTSS among parents whose children undergoing ECMO treatment.
Methods
Study design and participants
This cross-sectional study was conducted in five tertiary-level Grade A hospitals in Henan Province between January 2020 and July 2023. The study encompassed parents of children aged 0–12 undergoing Extracorporeal Membrane Oxygenation (ECMO) treatment, with specific inclusion and exclusion criteria set forth. Inclusion criteria comprised parents meeting the following conditions: (1) Having children aged 0–12 undergoing ECMO therapy, (2) Demonstrating adequate literacy and lacking communication barriers, and (3) Serving as the primary caregivers for their children under regular circumstances. Exclusion criteria, on the other hand, entailed the following conditions: (1) A history of mental illness or cognitive impairments, (2) Concurrently caring for another critically ill child at home, (3) Parental status for children undergoing ECMO for transplantation, and (4) Parental status for children afflicted with malignant tumors or severe infectious diseases.
This study received ethical approval from the Ethics Committee of Henan Children's Hospital and obtained informed consent from the study participants.
Procedures
The questionnaire was developed based on the consensus of ECMO application experts in the clinical field, covering four key dimensions. To refine the questionnaire, input was gathered from 11 experts in pediatric critical care to eliminate redundancy, enhance clarity, and ensure conciseness. A pilot study involving 31 participants was conducted, resulting in an overall Cronbach's α coefficient of 0.812, indicating robust internal consistency across the overall questionnaire.
The final questionnaire comprised the following sections: Demographic information about the participants, including age, gender, residence type, education level, employment status, income level, and more. The Knowledge dimension consisted of 9 questions, with responses scored as “very familiar” (2 points), “heard of it” (1 point), or “unfamiliar” (0 points). The Attitude dimension included 8 questions, utilizing a five-point Likert scale ranging from “very positive” (5 points) to “very negative” (1 point). The PTSS-related questionnaire contained 5 questions, with responses scored as option “a” (1 point) or option “b” (0 points), where a score above 2 indicated a potential PTSS condition14. Higher scores indicated better knowledge and more positive attitudes among the survey respondents.
Before official distribution, a small-scale pilot test involving 31 responses was conducted, resulting in a robust Cronbach's α coefficient of 0.766, indicative of strong internal consistency. Contact with hospitals was established through various means, including WeChat, phone calls, and email, with surveys administered to all eligible participants within the hospital settings. The distribution of questionnaires was overseen by eight research assistants who formed a survey team that underwent standardized training. These assistants provided consistent instructions, obtained informed consent, clarified survey procedures, guidelines, and confidentiality principles, and subsequently administered questionnaires in both digital and paper formats. For participants less familiar with electronic devices, paper questionnaires were provided, while others accessed the survey through online QR codes. The process was closely monitored by research assistants to discourage hasty completion. Participants independently completed the questionnaire if they understood the questions; otherwise, surveyors conducted face-to-face interviews, recording responses based on verbal input. After questionnaire completion, a rigorous examination of collected questionnaires was carried out. Data were entered twice by two individuals, with 20% of randomly selected samples subjected to re-entry to ensure data consistency and research data accuracy.
Statistical analysis
Statistical analysis was conducted using Stata 17.0 (Stata Corporation, Junior college Station, TX, USA). Quantitative variables were described using mean ± standard deviation (SD), and between-group comparisons were performed using t-tests or analysis of variance (ANOVA). Categorical variables were presented as n (%). Pearson correlation analysis was employed to assess the correlations between knowledge, attitude, and practice scores. Univariate variables with P < 0.05 were enrolled in multivariate regression. Hypotheses were validated using structural equation modeling (SEM). Hypotheses were validated using structural equation modeling (SEM). The hypotheses posited that Knowledge exerts a direct influence on Attitude and PTSS, Attitude directly impacts PTSS, and that residence, education, employment status, and monthly income directly affect Knowledge, Attitude, and PTSS. Two-sided P < 0.05 were considered statistically significant in this study.
Ethics approval and consent to participate
This work has been carried out in accordance with the Declaration of Helsinki (2000) of the World Medical Association. This study received ethical approval from the Ethics Committee of Henan Children's Hospital (2023-K-150) and obtained informed consent from the study participants.
Results
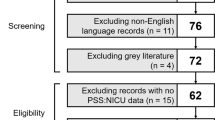
Initially, a total of 212 cases were collected in this study. The following cases were deleted: (1) 1 case with the age filled in as “330” and 1 case with the age filled in as “250”; (2) 8 cases in which the number of children in the family was filled in as 0 or none, but continued to answer the questions about children; (3) 1 case in which the number of children was filled in as “21”; the final valid questionnaire was 201 cases. Among these, 111 (55.22%) were female, with a mean age of 32 (range: 20–56) years, and most had one child. Additionally, 77 (38.31%) had completed junior college or undergraduate education, while 147 (73.13%) were employed. Of the participants, 75 (37.31%) indicated that their children required ECMO due to acute respiratory distress, and 183 (91.04%) had medical insurance coverage.
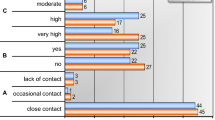
The median knowledge score was 3.00 (0–18) (possible range: 0–18), the mean attitude score was 27.00 ± 3.20 (possible range: 8—40), and the mean PTSS score was 3.50 ± 1.54 (possible range: 0—5). Parents with different genders were more likely to have different PTSS score (P = 0.050). Moreover, the knowledge, attitude, PTSS scores varied from those with different residence (P < 0.001, P < 0.001, and P = 0.004, separately), education (P < 0.001, P < 0.001, and P < 0.001, separately), employment status (P < 0.001, P < 0.001, and P = 0.007, separately), and monthly per capita income (P < 0.001, P < 0.001, and P = 0.010, separately) (Table 1).
No more than 10% chose option “Very familiar” for all knowledge section questions. The three questions with the highest number of participants choosing the “Heard of it” option were “Extracorporeal Membrane Oxygenation, colloquially referred to as “ECMO” or “artificial lung,” is a medical emergency device.” (K1) with 51.74%, “ECMO, as an effective adjunct for diseased hearts, can buy valuable time for further diagnosis and treatment of the heart.” (K5) with 36.82%, and “Complications of ECMO include bleeding, infection, central nervous system complications, thrombosis, and more.” (K8) with 36.82%. On the contrary, the three questions with the highest number of participants choosing the “Unfamiliar” option were “Whether it is a cardiac or respiratory disease, not all cases require VA (venous to arterial).” (K6) with 71.14%, “Internationally, ECMO can also be used in infants when necessary, and its effectiveness in infants is superior to that in adults.” (K7) with 71.14%, and “Due to ECMO punctures and catheter placement, local vascular damage may occur, resulting in long-term narrowing of blood vessels, possibly requiring subsequent vascular dilation procedures.” (K9) with 69.15% (Table 2).
In the context of ECMO's potential to extend treatment time for children (A1), it is notable that a significant majority of patients agree (56.93%). Examining the belief that all eligible patients should opt for ECMO (A2), 6.97% of respondents strongly agree, and 30.85% agree. Intriguingly, despite ECMO's high cost (A3), 13.43% of patients strongly agree, and 40.80% agree that it is a worthwhile option. Regarding the emotional impact of ECMO (A4), 10.95% of patients strongly agree, and 42.29% agree that ECMO instills great hope in them and their families. Conversely, concerns about potential harm following ECMO application (A5) are voiced by 11.44% of patients who strongly agree and 43.78% who agree. The understanding of ECMO's therapeutic function (A6) reveals that 6.47% of patients strongly agree, and 31.84% agree that it replaces respiratory or cardiopulmonary function rather than curing diseases. Furthermore, ECMO is not a panacea (A7), with 11.94% strongly agreeing and 51.24% agreeing that it should not be mythicized. Lastly, sentiments of regret about ECMO's limited promotion (A8) are expressed by 5.97% of patients who strongly agree and 31.34% who agree (Table 3).
Correlation analysis revealed significant positive associations between knowledge and attitude (r = 0.470, P < 0.001). Conversely, negative correlations were observed between knowledge and PTSS (r = −0.358, P < 0.001), as well as between attitude and PTSS (r = −0.323, P < 0.001) (Table 4).
Multivariate logistic regression analysis showed that junior high school education (OR = 28.260, 95% CI: 2.469–323.427, P = 0.007), high school/technical secondary school education (OR = 15.573, 95% CI: 2.589–93.680, P = 0.003), and the occupation of being a housewife (OR = 0.054, 95% CI: 0.005–0.548, P = 0.014) were independently associated with PTSS (Table 5).
Structural equation modeling (SEM) results provided insights into the relationships among variables. Residence had a direct impact on education (β = 0.973, P < 0.001), and education, in turn, directly influenced employment status (β = −0.372, P < 0.001), knowledge (β = 0.189, P < 0.001), attitude (β = 0.060, P = 0.047), and PTSS (β = −0.069, P = 0.003). Additionally, employment status exhibited direct effects on monthly income (β = −0.173, P < 0.001) and PTSS (β = −0.030, P = 0.017). Lastly, monthly income had a direct impact on knowledge (β = 0.130, P < 0.001), and knowledge, in turn, directly influenced attitude (β = 0.490, P < 0.001) (Fig. 1 and Supplementary Table 1).
Discussion
Parents of children undergoing ECMO treatment demonstrated insufficient knowledge, suboptimal attitudes, and were affected by PTSS. This study underscores the necessity for tailored educational initiatives aimed at parents with lower educational backgrounds. Furthermore, it emphasizes the importance of implementing psychosocial support programs to address parental PTSS during ECMO treatment. Healthcare providers should also take into account socioeconomic factors when developing communication and support strategies to enhance the overall experience and outcomes of parents involved in ECMO care.
In this study, the examination of parents of children undergoing ECMO revealed inadequate knowledge, suboptimal attitudes, and elevated levels of PTSS symptoms. The findings of this study are consistent with previous research, indicating that family members of patients undergoing ECMO treatment in the Intensive Care Unit (ICU) consistently experience stress12. This may be attributed to their insufficient knowledge and suboptimal attitudes towards PTSS, particularly when the patient is a child. These outcomes underscore the imperative to enhance clinical practices in ECMO care15. Effective strategies should prioritize educational initiatives and improved communication to bolster parental understanding and foster positive attitudes16. Additionally, integrating psychological support mechanisms to address PTSS symptoms is crucial17. Implementing these comprehensive approaches will enable healthcare teams to deliver more holistic and supportive care to families navigating the challenges of pediatric ECMO treatment.
The study results underscore the critical role of demographic factors in influencing the experiences of parents with children undergoing ECMO. These findings suggest that a one-size-fits-all approach to ECMO care and support is inadequate. Gender disparities, along with variations associated with residence, education, employment status, and income, point to the need for tailored interventions to address the unique needs and challenges of different parental groups18. Therefore, to enhance clinical practice, it is imperative to develop and implement interventions that consider these demographic factors as key determinants in delivering empathetic and effective care for parents facing the challenges of pediatric ECMO19. Such tailored approaches can contribute to improved emotional well-being and overall outcomes for these families20.
The study revealed a notable deficiency in participants' knowledge about ECMO, with less than 10% indicating a “Very familiar” level of understanding across all knowledge section questions. Questions concerning fundamental ECMO concepts received the highest recognition, while those addressing more nuanced aspects of ECMO care generated significant unfamiliarity among participants. This highlights the necessity for comprehensive educational programs aimed at bridging this knowledge gap among healthcare professionals21. Such programs should cover both foundational and specialized ECMO topics to promote better-informed clinical practice and ultimately enhance patient outcomes.
Patient attitudes towards ECMO revealed important considerations for enhancing clinical practice. The generally positive outlook on ECMO's potential benefits and extended treatment time underscores the importance of comprehensive patient education, emphasizing both its advantages and limitations18,22. Patients' willingness to consider ECMO as a viable option despite its cost highlights the necessity of transparent discussions about healthcare expenses and financial considerations23. However, concerns about potential harm following ECMO application call for improved pre-ECMO counseling and support. These findings emphasize the pivotal role of communication and patient-centered care in refining ECMO clinical practices, ensuring they align with patients' preferences and needs24,25,26.
The analysis revealed significant relationships between key variables. Knowledge and attitude were positively correlated, indicating that as knowledge increases, attitudes tend to become more positive27. Conversely, negative correlations were observed between knowledge and PTSS, as well as between attitude and PTSS, suggesting that parents with more knowledge and positive attitudes may experience lower levels of PTSS28,29. SEM results showed that factors like residence influenced education, which in turn affected employment status, knowledge, attitude, and PTSS30. Employment status had direct effects on monthly income and PTSS. Additionally, monthly income influenced knowledge, which in turn affected attitude. These findings highlight the interconnectedness of various factors in shaping parental experiences and attitudes regarding pediatric ECMO, emphasizing the need for a comprehensive and tailored approach to support and education for parents31,32.
Theoretical implications
The findings of this study contribute to the theoretical understanding of parental experiences and responses to stress in the context of pediatric medical interventions, specifically ECMO treatment. By identifying associations between education levels, employment status, and PTSS among parents, this research underscores the importance of socio-demographic factors in shaping parental psychological well-being. Additionally, the observed relationships between knowledge, attitude, and PTSS highlight the potential pathways through which parental understanding and perception of medical procedures may influence their emotional responses. These theoretical insights provide a basis for further research into the mechanisms underlying parental adaptation to pediatric medical crises and inform the development of targeted interventions to support parental coping and adjustment.
Empirical implications
The empirical findings of this study offer valuable insights into the knowledge, attitude, and PTSS among parents of children undergoing ECMO treatment. The identification of specific demographic factors associated with elevated PTSS, such as lower education levels and occupation as housewives, provides empirical evidence for the differential impact of socio-economic status on parental psychological outcomes in this population. Moreover, the application of logistic regression and structural equation modeling techniques enhances our understanding of the complex interplay between socio-demographic variables, parental perceptions, and psychological distress. These empirical findings contribute to the evidence base for tailored interventions aimed at improving parental well-being and family functioning during pediatric medical crises.
Limitations
This study had some limitations. First, the study's cross-sectional design limits our ability to establish causality or track changes in knowledge, attitude, and PTSS over time33. Longitudinal research could provide a more comprehensive understanding of how these factors evolve during the ECMO experience. Second, the data collection method, which relied on a web-based survey, may introduce selection bias as it excludes individuals without internet access or those who might not have participated due to various reasons. Additionally, self-report questionnaires are subject to response bias, as participants may provide socially desirable responses or recall inaccuracies.
Recommendations
Based on the findings and limitations of this study, several recommendations emerge for future research and clinical practice. Longitudinal studies employing mixed-methods approaches are warranted to investigate the longitudinal trajectories of parental adjustment and identify modifiable factors contributing to resilience or vulnerability. Clinically, healthcare professionals should implement routine screening for parental PTSS and provide accessible psychosocial support services tailored to the needs of parents, particularly those with lower education levels or limited social support networks. Educational interventions aimed at enhancing parental knowledge and fostering positive attitudes towards medical procedures should be integrated into the ECMO care protocol to empower parents and alleviate distress. Collaborative efforts between researchers, healthcare providers, and policymakers are essential to address the multifaceted needs of parents facing pediatric medical crises and promote optimal family-centered care.
In conclusion, parents of children undergoing ECMO often lack sufficient knowledge, exhibit suboptimal attitudes, and may experience PTSS. To enhance their experience, we recommend comprehensive education, with a focus on parents with lower education levels. Addressing parental PTSS through psychosocial support and regular screening is crucial. Integrating socioeconomic factors into support strategies can tailor care to individual needs, leading to improved outcomes for parents and their children during ECMO treatment.
Data availability
All data generated or analysed during this study are included in this published article and its supplementary information files.
References
Xu, L. et al. The challenges of apnea tests in the determination of brain death in child patient on extracorporeal membrane oxygenation. Front. Pediatr. 8, 358 (2020).
Jing, Y. et al. A phased intervention bundle to decrease the mortality of patients with extracorporeal membrane oxygenation in intensive care unit. Front. Med. 9, 1005162 (2022).
Boyle, K. et al. Neurologic outcomes after extracorporeal membrane oxygenation: A systematic review. Pediatr. Crit. Care Med. 19, 760–766 (2018).
Drop, J. G. et al. Use of rotational thromboelastometry to predict hemostatic complications in pediatric patients undergoing extracorporeal membrane oxygenation: A retrospective cohort study. Res. Pract. Thromb. Haemost. 5, e12553 (2021).
Aristidou, L., Mpouzika, M., Papathanassoglou, E. D. E., Middleton, N. & Karanikola, M. N. K. Association between workplace bullying occurrence and trauma symptoms among healthcare professionals in Cyprus. Front. Psychol. 11, 575623 (2020).
Camporesi, A. et al. The parental psychological distress caused by separation from their critically ill child during the COVID-19 pandemic: A tale of two cities. Front. Pediatr. 10, 909210 (2022).
Willinger, Y. & Turgeman, G. Interleukine-17 modulates neurogenesis and behavior following exposure to trauma in mice. Cells 11, 343 (2022).
Khalid, A. et al. Promoting health literacy about cancer screening among Muslim immigrants in Canada: Perspectives of imams on the role they can play in community. J. Prim. Care Community Health. 13, 21501319211063052 (2022).
Koni, A. et al. A cross-sectional evaluation of knowledge, attitudes, practices, and perceived challenges among Palestinian pharmacists regarding COVID-19. SAGE Open Med. 10, 20503121211069280 (2022).
Shubayr, M. A., Kruger, E. & Tennant, M. Oral health providers’ views of oral health promotion in Jazan, Saudi Arabia: A qualitative study. BMC Health Serv. Res. 23, 214 (2023).
Hoehn, K. S. Posttraumatic stress and technology: Do extracorporeal membrane oxygenation programs have an ethical obligation to provide ongoing psychological support for parents?*. Pediatr. Crit. Care Med. 15, 180–181 (2014).
Onrust, M. et al. Coping strategies, anxiety and depressive symptoms in family members of patients treated with extracorporeal membrane oxygenation: A prospective cohort study. Heart Lung. 52, 146–151 (2022).
Alonso-Fernandez-Gatta, M. et al. Post-traumatic stress disorder symptoms after veno-arterial extracorporeal membrane oxygenator support. Heart Lung. 50, 775–779 (2021).
Prins, A. et al. The primary care PTSD screen for DSM-5 (PC-PTSD-5): Development and evaluation within a veteran primary care sample. J. Gen. Intern. Med. 31, 1206–1211 (2016).
Sniderman, J., Monagle, P., Annich, G. M. & MacLaren, G. Hematologic concerns in extracorporeal membrane oxygenation. Res. Pract. Thromb. Haemost. 4, 455–468 (2020).
Xiong, C., Chen, X., Zhao, X. & Liu, C. Patient satisfaction and gender composition of physicians—A cross-sectional study of community health services in Hubei, China. BMC Health Serv. Res. 18, 217 (2018).
Yeh, M. S. L. et al. Subjective and objective sleep quality in young women with posttraumatic stress disorder following sexual assault: A prospective study. Eur. J. Psychotraumatol. 12, 1934788 (2021).
Xiao, X. et al. Assessment of radiation risk perception and interest in tritiated water among returnees to and evacuees from Tomioka Town within 20 km of the Fukushima Daiichi Nuclear Power Plant. Int. J. Environ. Res. Public Health. 20, 2690 (2023).
Jeppesen, P. et al. Effectiveness of transdiagnostic cognitive-behavioral psychotherapy compared with management as usual for youth with common mental health problems: A randomized clinical trial. JAMA Psychiatry. 78, 250–260 (2021).
Nordfalk, J. M., Holmøy, T., Thomas, O., Nylenna, M. & Gulbrandsen, P. Training physicians in providing complex information to patients with multiple sclerosis: A randomised controlled trial. BMJ Open. 12, e049817 (2022).
Como, D. H., Floríndez, L. I., Tran, C. F., Cermak, S. A. & Stein Duker, L. I. Examining unconscious bias embedded in provider language regarding children with autism. Nurs. Health Sci. 22, 197–204 (2020).
Park, H. & Cho, H. Effects of a self-directed clinical practicum on self-confidence and satisfaction with clinical practicum among South Korean nursing students: A mixed-methods study. Int. J. Environ. Res. Public Health. 19, 5231 (2022).
Yu, W., Liu, X., Zhao, F., Li, M. & Zhang, L. Control of unreasonable growth of medical expenses in public hospitals in Shanghai, China: A multi-agent system model. BMC Health Serv. Res. 20, 490 (2020).
Chen, L., Zhang, D. & Hou, M. The influence of perceived social presence on the willingness to communicate in mobile medical consultations: Experimental study. J. Med. Internet Res. 24, e31797 (2022).
Cho, M. Evaluating Therapeutic Healthcare Environmental Criteria: Architectural Designers’ Perspectives. Int. J. Environ. Res. Public Health. 20, 1540 (2023).
Nourein, A. A. E. et al. Comparative study of attitudes towards communication skills learning between medical and dental students in Saudi Arabia. Int. J. Environ. Res. Public Health. 18, 128 (2020).
Ng, T. K. C., Lo, M. F., Fong, B. Y. F. & Yee, H. H. L. Predictors of the intention to use traditional Chinese medicine (TCM) using extended theory of planned behavior: A cross-sectional study among TCM users in Hong Kong. BMC Complement. Med Ther. 22, 113 (2022).
deRoon-Cassini, T. A. et al. Circulating endocannabinoids and genetic polymorphisms as predictors of posttraumatic stress disorder symptom severity: Heterogeneity in a community-based cohort. Transl. Psychiatry. 12, 48 (2022).
Rizkalla, N. & Segal, S. P. Trauma during humanitarian work: The effects on intimacy, wellbeing and PTSD-symptoms. Eur. J. Psychotraumatol. 10, 1679065 (2019).
El-Khodary, B., Samara, M. & Askew, C. Traumatic events and PTSD among Palestinian children and adolescents: The effect of demographic and socioeconomic factors. Front. Psychiatry. 11, 4 (2020).
Ball, G. D. C. et al. A multi-center, randomized, 12-month, parallel-group, feasibility study to assess the acceptability and preliminary impact of family navigation plus usual care versus usual care on attrition in managing pediatric obesity: a study protocol. Pilot Feasib. Stud. 9, 14 (2023).
Timakum, T., Xie, Q. & Song, M. Analysis of E-mental health research: Mapping the relationship between information technology and mental healthcare. BMC Psychiatry. 22, 57 (2022).
Musa, K. I. & Keegan, T. J. The change of Barthel Index scores from the time of discharge until 3-month post-discharge among acute stroke patients in Malaysia: A random intercept model. PLoS ONE 13, e0208594 (2018).
Funding
This work was supported by the 2023 Henan Province medical science and technology research plan joint construction project (LHGJ20230579) and 2020 Henan Province medical science and technology research plan joint construction project (LHGJ20200664).
Author information
Authors and Affiliations
Contributions
Y.S. and C.S. carried out the studies, participated in collecting data, and drafted the manuscript. H.W. and L.L. performed the statistical analysis and participated in its design. Y.W. and Y.S. participated in acquisition, analysis, or interpretation of data and draft the manuscript. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Sun, Y., Wang, H., Wu, Y. et al. Parents' knowledge and attitudes towards extracorporeal membrane oxygenation and their post-traumatic stress symptoms. Sci Rep 14, 10700 (2024). https://doi.org/10.1038/s41598-024-60880-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-024-60880-3
Keywords
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.