Abstract
For any given level of overall adiposity, individuals vary considerably in fat distribution. The inherited basis of fat distribution in the general population is not fully understood. Here, we study up to 38,965 UK Biobank participants with MRI-derived visceral (VAT), abdominal subcutaneous (ASAT), and gluteofemoral (GFAT) adipose tissue volumes. Because these fat depot volumes are highly correlated with BMI, we additionally study six local adiposity traits: VAT adjusted for BMI and height (VATadj), ASATadj, GFATadj, VAT/ASAT, VAT/GFAT, and ASAT/GFAT. We identify 250 independent common variants (39 newly-identified) associated with at least one trait, with many associations more pronounced in female participants. Rare variant association studies extend prior evidence for PDE3B as an important modulator of fat distribution. Local adiposity traits (1) highlight depot-specific genetic architecture and (2) enable construction of depot-specific polygenic scores that have divergent associations with type 2 diabetes and coronary artery disease. These results – using MRI-derived, BMI-independent measures of local adiposity – confirm fat distribution as a highly heritable trait with important implications for cardiometabolic health outcomes.
Similar content being viewed by others
Introduction
Overall fat mass and fat distribution represent two correlated but distinct axes of variation that determine the health impacts of adipose tissue. Individuals with high body mass index (BMI)—defining obesity—are at elevated risk of type 2 diabetes and cardiovascular events, but increased cardiometabolic risk has also been noted in individuals with the same BMI when fat is disproportionally depleted in more favorable gluteofemoral fat depots and deposited instead in visceral and ectopic fat depots1,2,3,4,5. An extreme example of this paradigm occurs in Mendelian lipodystrophies, such as those caused by missense mutations in the LMNA and PPARG genes6,7,8,9,10. By contrast, the genetic architecture of more subtle variation in fat distribution across the general population warrants further attention.
In general, prior studies aiming to elucidate common genetic variation contributing to fat distribution can be categorized into three study types: (1) genome-wide association studies (GWAS) on anthropometric proxies of fat distribution, (2) studies combining GWAS summary statistics of metabolic and anthropometric traits, and (3) GWASs on imaging-based measures of fat distribution. The first type has been spearheaded by the Genetic Investigation of ANthropometric Traits (GIANT) consortium and others, leading to the discovery of over 300 loci associated with waist-to-hip ratio adjusted for BMI (WHRadjBMI) in an analysis of nearly 700,000 individuals11,12. Another recent GWAS aimed to examine fat distribution using estimates of body composition based on stepping on a scale equipped with impedance technology, known to be reasonably accurate for total fat volume but less so for fat distribution13,14,15. Despite the considerable value of these studies, a central limitation is an unclear relationship between each anthropometric trait and each fat depot of biological interest—for example, an increase in WHRadjBMI could be capturing increased visceral adipose tissue (VAT; around the abdominal organs), increased abdominal subcutaneous adipose tissue (ASAT; abdominal fat under the skin), decreased gluteofemoral adipose tissue (GFAT; hip and thigh fat), or some combination of these perturbations16,17. Variation in WHRadjBMI could also reflect variation in muscle and bone mass, rather than adipose tissue burden.
A second category of studies has aimed to gain further resolution into anthropometric loci by combining summary statistics of metabolic and anthropometric traits, generating clusters of metabolically favorable and unfavorable loci18,19,20,21,22,23. These studies have succeeded in establishing a common variant basis for metabolically distinct fat depots, with seminal work demonstrating that an insulin resistance polygenic score is associated with lower hip circumference in the general population, and that individuals with familial partial lipodystrophy type 1 (FPLD1) have a higher burden of this polygenic score19. Along with their reliance on anthropometric proxies of fat distribution, these studies are limited by their inclusion requirement of nominal significance across multiple metabolic traits which is likely leading to only a fraction of the genetic architecture of fat distribution being described.
Finally, the third category of studies performed GWASs on measurements derived from body imaging24,25,26,27,28,29. These include GWASs of CT-quantified VAT and ASAT in nearly 20,000 individuals, GWASs on MRI-quantified VAT and ASAT, and a GWAS of a predicted VAT trait using several anthropometric traits trained on over 4000 DEXA-measured VAT values26,27,28,29. These studies have been important for translating insights from anthropometric and metabolic trait GWASs to image-derived measurements of the fat depots of interest, but have been limited by (1) the absence of GFAT, which appears to have a metabolically protective role in contrast to VAT and ASAT, and frequently (2) a reliance on raw, unadjusted fat depot metrics which are highly correlated with both each other and BMI.
In this study, we investigate the common and rare variant genetic architecture of three fat depots as quantified by MRI in up to 38,965 UK Biobank participants. Beyond study of raw VAT, ASAT, and GFAT volumes, we analyze six measures that better reflect local adiposity and fat distribution: VAT adjusted for BMI and height (VATadj), ASATadj, GFATadj, VAT/ASAT, VAT/GFAT, and ASAT/GFAT. We show that these local adiposity traits (1) highlight depot-specific genetic architecture, (2) reflect sex-dimorphism previously appreciated with anthropometric traits, and (3) can be used to construct depot-specific polygenic scores that have divergent associations with type 2 diabetes and coronary artery disease. This study is to our knowledge the largest imaging-based study to date to disentangle the genetic architecture of different fat depots—including GFAT, a fat depot that appears to confer protection from adverse cardiometabolic health5,30.
Results
VAT, ASAT, and GFAT volumes were quantified in participants of the UK Biobank using a deep learning model trained on body MRI imaging, as previously described (Fig. 1, Supplementary Fig. 1, and Supplementary Table 1)5. Among those with MRI-quantified fat depot volumes, 39,076 had genotyping array data available, enabling common variant association studies in up to 38,965 participants after quality control (“Methods”). Mean age in the genotyped cohort was 64.5 years, 51% were female, and 87% were of white British ancestry as previously defined in this study (Supplementary Data 1 and 2). As expected, significant sex differences in fat depot volumes were observed—male participants had higher mean VAT volume (5.0 vs. 2.6 L), while female participants had higher ASAT volume (7.9 vs. 5.9 L) and GFAT volume (11.3 vs. 9.3 L)31,32.
(Top left) Three female participants from the UK Biobank with similar age (67–70 years) and similar overweight BMI (27.6–28.6 kg/m2) with highly discordant fat distributions (right) Manhattan plots for sex-combined GWASs with VAT adjusted for BMI and height (VATadj), ASATadj, and GFATadj. Lead SNPs are described in Supplementary Data 3. (Bottom left) Overlap between VATadj, ASATadj, and GFATadj loci denoted by the nearest gene; lead SNPs of two traits in high LD (R2 ≥ 0.1) were plotted in the intersection. GWAS significance at a commonly used threshold of p < 5 × 10−8 was required for inclusion in the Venn diagram.
Six additional adiposity traits—designed to better capture local adiposity—were additionally computed for each individual: VATadj, ASATadj, GFATadj were computed by taking sex-specific residuals against age, age squared, BMI, and height, while VAT/ASAT, VAT/GFAT, and ASAT/GFAT were computed by taking ratios between each pair of fat depots without additional residualization (Supplementary Fig. 5). We tested VATadj, ASATadj, and GFATadj for possible collider bias with BMI or height and found minimal or no evidence of such bias for the majority of genome-wide significant loci (Supplementary Methods, Supplementary Figs. 2–4, and Supplementary Tables 2–5). For example, 87% of VATadj, 86% of ASATadj, and 98% of GFATadj genome-wide significant loci had stronger effect size for the unadjusted fat depot volume compared to BMI, comparable to the 90% of WHRadjBMI loci that met analogous criteria in a recent meta-analysis12.
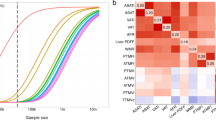
In contrast to VAT, ASAT, and GFAT volumes which were highly correlated with BMI (Pearson r ranging from 0.77–0.88), VATadj, ASATadj, GFATadj, and VAT/ASAT were nearly independent of BMI (Pearson r ranging from 0–0.18), while VAT/GFAT (Pearson r = 0.42) and ASAT/GFAT (Pearson r = 0.56) displayed attenuated correlations with BMI (Fig. 2 and Supplementary Fig. 6A, B). These six derived adiposity traits provided useful, less BMI-dependent metrics for downstream analyses.
Local adiposity traits are highly heritable and genetically distinct from each other
To quantify the inherited component to each of these nine adiposity traits, we used the BOLT-REML algorithm to estimate SNP-heritability. Heritability estimates for VAT, ASAT, and GFAT ranged from 0.31–0.36 (standard error (SE) = 0.01), comparable to that observed for BMI in the same individuals (hg2: 0.31, SE = 0.02)) (Supplementary Table 6). BMI-adjusted fat depots and fat depot ratios tended to have higher heritability compared to unadjusted fat depots and BMI (hg2 ranging from 0.34–0.41, SE = 0.01–0.02). In contrast, WHRadjBMI, an anthropometric proxy for local adiposity, was less heritable than these traits (hg2: 0.21, SE = 0.01). In sex-stratified analyses, most adiposity traits were more heritable in females as compared to males, with the greatest heritability across all analyses for GFATadj in females (hg2: 0.52, SE = 0.03).
To study the genetic correlations (rg) between the adiposity and related anthropometric traits, we used LD-score regression33,34. Results were generally consistent with observational correlations—raw VAT, ASAT, and GFAT volumes were highly genetically correlated with BMI (rg ranging from 0.66–0.82), while the three adjusted fat depots, VAT/ASAT, and VAT/GFAT exhibited low genetic correlation with BMI (rg ranging from −0.16–0.28) (Fig. 2 and Supplementary Fig. 7A, B). In sex-combined analyses, VATadj, ASATadj, and GFATadj were genetically correlated with their unadjusted counterparts (rg ranging from 0.45–0.59), but nearly independent of the other two fat depots (rg ranging from –0.24–0.15), suggesting that adjusted-for-BMI traits can enable fat depot-specific genetic analyses. Finally, WHRadjBMI exhibited positive genetic correlations with VATadj (rg: 0.65) and ASATadj (rg: 0.25), and a negative genetic correlation with GFATadj (rg: −0.29), consistent with the perturbations needed in each fat depot to drive a change in WHRadjBMI.
Common variant architecture of adiposity traits
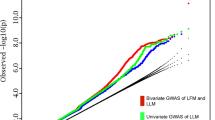
We next conducted GWAS for each of the nine adiposity traits—VAT, ASAT, GFAT, VATadj, ASATadj, GFATadj, VAT/ASAT, VAT/GFAT, and ASAT/GFAT—in sex-combined and sex-stratified groups using BOLT-LMM. After genotyping quality control, we tested associations with 11.5 million imputed SNPs with minor allele frequency (MAF) > 0.005. Across all 27 association studies, 250 loci were associated with at least one adiposity trait at a p value threshold of 5 × 10−8 (Supplementary Data 3). If a more stringent genome-wide significance threshold of 5 × 10−9 had been used, we would have identified 136 loci, or 85 loci at the most conservative Bonferroni-corrected threshold of 5 × 10−9/27 = 1.9 × 10−10. Of the 250 loci across all adiposity traits, 39 were newly-identified (defined as R2 < 0.1 with all genome-wide significant associations with prior adiposity and relevant anthropometric traits in the GWAS catalog) (Table 1; Methods; and Supplementary Data 4)35. Of these 39 loci, 35 have been previously associated with at least one cardiometabolic trait with nominal significance (p < 0.05) (Supplementary Table 7). Consistent with heritability estimates, the greatest number of loci were identified in association with GFATadj (54 lead SNPs), while the fewest were identified in association with ASAT (6 lead SNPs). The greatest genomic inflation parameter (λGC) was observed with GFATadj (λGC: 1.14)—the LD-score regression intercept was 1.05, consistent with polygenicity rather than significant population structure (Supplementary Table 8)33.
We began by investigating the genetic architecture of VAT, ASAT, and GFAT volumes (Supplementary Fig. 8). All three traits shared a genome-wide significant association with an intronic FTO variant (rs56094641) previously associated with childhood and adult obesity36,37,38. ASAT harbored the most significant association with this locus (p = 1.3 × 10−22), followed by GFAT (p = 1.2 × 10−12), and finally VAT (p = 3.3 × 10−10), reflecting the strength of observational and genetic correlation of each fat depot with BMI. Given observational and genetic evidence that a large component of each fat depot volume trait is accounted for by BMI—or “overall adiposity”—we focused further common variant analyses to the three adjusted-for-BMI-and-height measures and three fat depot ratios, aiming to study the genetic architecture of “local adiposity.”
For VATadj, 30 genome-wide significant associations were identified (p < 5 × 10−8) (Fig. 1 and Supplementary Fig. 9). The two most significantly associated variants were an intronic CDCA2 variant (rs11992444; p = 1.3 × 10−29) previously associated with WHRadjBMI and serum triglycerides, and an intronic PEPD variant (rs10406327; p = 3.3 × 10−24) previously associated with waist circumference adjusted for BMI (WCadjBMI) and type 2 diabetes12,39,40,41. Newly-identified loci in association with VATadj included an intronic GPR158 variant (rs1329254; p = 1.4 × 10−8), and an intronic ARHGEF3 variant exclusively in females (rs1500714; p = 1.8 × 10−8). Prior work has similarly noted female-specific effects of variation in this gene including an association with postmenopausal osteoporosis in humans and Arhgef3-KO mice being found to have improved muscle regeneration following injury, with an enhanced rate in females, although the role of this gene on fat distribution is uncertain42,43.
The most statistically significant association with ASATadj was an intronic ADAMTSL3 variant (rs768397327; p = 2.2 × 10−17), which was in near-perfect linkage disequilibrium (R2 = 0.97) with another intronic ADAMTSL3 variant (rs11856122) previously associated with bioelectrical impedance-derived arm fat ratio, leg fat ratio, and trunk fat ratio (Fig. 1 and Supplementary Fig. 10)13. Another genome-wide significant signal was observed with an intronic PPARG variant (rs527620413). Rare variants in PPARG have previously been associated with familial partial lipodystrophy6,7. The minor alleles at this locus (MAF = 0.12), which additionally consisted of rs17036328 and rs71304101 (R2 > 0.90), were associated with increased ASATadj (rs527620413; beta = 0.071; p = 6.8 × 10−11), increased GFATadj (rs71304101; beta = 0.062; p = 1.7 × 10−9), decreased VAT/ASAT ratio (rs17036328; beta = −0.080; p = 5.8 × 10−15), and decreased VAT/GFAT ratio (rs17036328; beta = −0.058; p = 2.4 × 10−8). These three SNPs are also in high LD (R2 ≥ 0.94) with rs1801282, a missense variant in PPARG previously associated with reduced risk of type 2 diabetes44,45,46. These data suggest that common variation at PPARG can lead to adiposity variation along the lipodystrophy axis—for this locus, the minor alleles associated with a pattern of favorable adiposity. FST is another gene that promotes adipogenesis and may have a causal role in insulin resistance—an intronic variant in FST (rs55744247) associated with ASATadj (p = 5.1 × 10−10), but not VATadj (p = 0.80) or GFATadj (p = 0.25)47. Finally, a newly-identified intronic DMRT2 variant (rs6474550; p = 1.3 × 10−9) associated with ASATadj. In a study investigating fat depot-specific transcriptome signatures before and after exercise, DMRT2 was one of three genes with higher expression in ASAT vs. GFAT both before and after exercise48.
The top GFATadj signal was an intronic RSPO3 variant (rs72959041; p = 3.2 × 10−32) that has previously been shown to be a top signal for WHRadjBMI (Fig. 1 and Supplementary Fig. 11)12. Recent work clarified this SNP as the causal variant at the locus and suggested that the minor allele concurrently reduces leg fat mass and increases android fat mass49. Our results confirm and further clarify these findings—the minor allele (MAF = 0.05) associated with marked reduction of GFATadj (beta = −0.195; p = 3.2 × 10−32) and increased of VATadj (beta = 0.118; p = 7.8 × 10−13), but a nonsignificant effect on ASATadj (beta = −0.029; p = 0.09). Three independent intronic COBLL1 variants (R2 < 0.1) were associated with GFATadj (rs13389219; p = 3.0 × 10−23, rs3820981; p = 1.5 × 10−12, rs34224594; p = 2.8 × 10−9), but not VATadj (pmin = 0.009) or ASATadj (pmin = 2.7 × 10−3). One of these variants (rs13389219) is in LD with another intronic COBLL1 variant (rs6738627) which has previously been implicated in a metabolically healthy obesity phenotype characterized by increased HDL cholesterol and reduced triglycerides despite increased body fat percentage50. In this study, aligning rs13389219 to the BMI-increasing direction (beta = 0.011, p = 7.3 × 10−3) revealed a concurrent increase in GFATadj (beta = 0.073), consistent with a metabolically healthy fat depot shift. Finally, a GFATadj association was observed at an intronic PDGFC variant (rs6822892; p = 8.0 × 10−13)—PDGFC was recently prioritized as a candidate causal gene for insulin resistance in human preadipocytes and adipocytes47.
Several associations were exclusive to GWASs of fat depot ratios (Supplementary Figs. 12–14). A missense variant in ACVR1C significantly reduced VAT/GFAT ratio (rs55920843; MAF = 0.01; beta = −0.18; p = 1.9 × 10−8). Prior work demonstrated that sequence variation in ACVR1C—including this variant—reduces WHRadjBMI and risk of type 2 diabetes51. Another missense variant in ACVR1C was nominally associated with reduced VAT/GFAT ratio, strengthening the importance of this gene (rs56188432 (p.Ile195Thr); beta = −0.21, p = 0.006) (Supplementary Data 5). Finally, a newly-identified association was present between VAT/GFAT ratio and a missense variant in SERPINA1 (rs28929474; MAF = 0.02; beta = −0.16; p = 4.8 × 10−10). Homozygous carriers of this variant are known to harbor alpha-1-antitrypsin deficiency, and heterozygous carriers have higher serum ALT and increased risk of cirrhosis51,52. Interestingly, this missense variant has also been associated with reduced risk of type 2 diabetes (odds ratio: 0.90, p = 5.9 × 10−6) and coronary artery disease (odds ratio: 0.88, p = 9.4 × 10−9)41,53. The present association with reduced VAT/GFAT ratio suggests that a shift toward a metabolically healthy fat distribution could partially explain a reduced risk of cardiometabolic disease. In a large meta-analysis, this SERPINA1 variant had only a nominally significant association with waist-to-hip ratio (beta = −0.03, p = 3.4 × 10−4)—the closest anthropometric correlate of VAT/GFAT ratio—highlighting the utility of image-derived phenotypes for this discovery12.
Gluteofemoral adiposity signal classification
We aimed to categorize genetic loci associated with gluteofemoral adiposity—postulated to be metabolically protective—into distinct clusters. Starting with the 250 lead SNPs that were associated (p < 5 × 10−8) with any of the nine adiposity traits in this study, we selected 101 LD-pruned (r2 = 0.1) SNPs that were nominally associated (p < 0.05) with GFATadj. Each SNP was aligned to the GFATadj increasing direction. We used Bayesian non-negative matrix factorization (bNMF)—a soft clustering approach—with 32 cardiometabolic traits including anthropometric traits (e.g., BMI, body fat percentage), lipid traits (e.g., triglycerides, HDL-cholesterol, and total cholesterol), and diabetes-related traits (e.g., glucose, hemoglobin A1C) to identify clusters (Supplementary Data 6).
In all 100 iterations, the data converged to three clusters (Supplementary Data 7). The most strongly weighted traits for the first cluster included increased HDL-cholesterol, decreased serum triglycerides, decreased hemoglobin A1C, and decreased alanine aminotransferase, consistent with a metabolically healthier fat distribution. Top loci in this cluster included several well-known associations with WHRadjBMI and insulin resistance including COBLL1, RSPO3, PPARG, and DNAH1012,47,54,55. A second cluster appeared to be related to inflammatory pathways, with top loci including HLA-DRB5, HLA-B, and MAFB—MAFB has previously been implicated as a regulator of adipose tissue inflammation56. Strongly weighted traits in this cluster included decreased aspartate aminotransferase, decreased total cholesterol, and decreased C-reactive protein. The third and final cluster appeared to reflect the interplay between hepatocyte biology and fat distribution with top loci including a missense variant in SERPINA1 and SHBG—the former is known to cause alpha-1-antitrypsin deficiency and has been previously associated with increased ALT and cirrhosis, and sex-hormone binding globulin is synthesized by hepatocytes and is reduced in patients with non-alcoholic fatty liver disease57,58. Strongly weighted traits in this cluster included increased albumin, increased sex-hormone binding globulin, and increased total protein.
To test the robustness of these results, we performed two sensitivity analyses. First, we performed clustering using 85 LD-pruned SNPs nominally associated (p < 0.05) with unadjusted GFAT. The three aforementioned clusters were reproduced along with a fourth cluster representing overall adiposity—the top locus in this cluster was FTO and the most strongly weighted trait was increased BMI (Supplementary Data 8). Finally, we performed one additional clustering analysis of the same 101 LD-pruned SNPs for GFATadj, this time including VATadj and ASATadj as clustering traits alongside the 32 previously used cardiometabolic traits, resulting in a nearly identical set of three clusters (Supplementary Data 9).
Sex heterogeneity in genetic associations with local adiposity traits
Given prior work has noted significant sex heterogeneity in the genetic basis of anthropometric traits, we next tested for such heterogeneity for each of the six local adiposity traits (VATadj, ASATadj, GFATadj, VAT/ASAT, VAT/GFAT, and ASAT/GFAT)11,12,55,59. Genetic correlations between sex-stratified summary statistics indicated overall high correlation between traits, with rg somewhat higher for VATadj (rg = 0.87) as compared to ASATadj or GFATadj (rg = 0.80 and 0.79 respectively) (Supplementary Table 9). We next tested for sex-dimorphism across loci that were genome-wide significant for either sex-combined or sex-stratified analyses for each local adiposity trait (Fig. 3, Supplementary Fig. 15, and Supplementary Data 10). Three of 34 VATadj loci (9%), six of 27 ASATadj loci (22%), and six of 65 GFATadj (9%) showed significant sex dimorphism (pdiff <0.05/220 independent loci-trait pairs tested = 2.3 × 10−4). The majority of these signals were driven by a greater magnitude of effect in female participants, which is consistent with prior investigations of WHRadjBMI12,55. Across all six local adiposity traits, 26 trait-loci associations were only genome-wide significant in females, while 9 loci were only genome-wide significant in males.
For each adiposity trait, independent loci that were associated with the trait in either sex-combined or sex-stratified analyses are plotted (Supplementary Data 10). Thirty-four such loci are plotted for VATadj, 27 for ASATadj, and 65 for GFATadj. Loci colored black were genome-wide significant (p < 5 × 10−8) in sex-combined analysis, blue loci were significant for males, but neither females nor sex-combined, and red loci were significant for females, but neither males nor sex-combined. pdiff corresponds to the “calcpdiff” function in EasyStrata comparing SNP effects in males and females (Methods). Across six adiposity traits (VATadj, ASATadj, GFATadj, VAT/ASAT, VAT/GFAT, and ASAT/GFAT), 220 unique loci-trait pairs were tested for sex heterogeneity (Supplementary Fig. 15), so a Bonferroni-corrected significance threshold of pdiff < 0.05/220 = 2.3 × 10−4 was set.
Overlap of local adiposity traits with WHRadjBMI findings
To investigate the added value of precisely quantifying fat depots with MRI in a smaller number of individuals as compared to WHRadjBMI in a larger cohort, we studied the effects of 345 loci identified in the most recent WHRadjBMI meta-analysis of up to 694,649 individuals on VATadj, ASATadj, and GFATadj (Fig. 4 and Supplementary Data 11)12. Of the 345 loci, 10 (3%) achieved genome-wide significance in association with VATadj (p < 5 × 10−8), 2 with ASATadj (0.6%), and 14 (4%) with GFATadj. A unit increase in WHRadjBMI might be expected to be reflecting a unit increase in VATadj or ASATadj, or a unit decrease in GFATadj. We quantified how often a locus was discordant from this pattern (e.g., a unit increase in WHRadjBMI corresponding to a unit decrease in VATadj), excluding loci where the fat depot effect size was smaller in magnitude than the SE. Fifteen of 242 loci (6%) were VATadj-discordant, 71 of 166 loci (43%) were ASATadj-discordant, and 22 of 231 loci (10%) were GFATadj-discordant (Supplementary Data 11).
In total, 345 of the 346 index SNPs associated with WHRadjBMI in a recent meta-analysis from the GIANT consortium were available in the studied cohort12. Effect sizes of VATadj, ASATadj, and GFATadj are plotted against the effect size for WHRadjBMI as reported in the cited study (Supplementary Data 11). Betas and p values for VATadj, ASATadj, and GFATadj correspond to the BOLT-LMM association p values computed in this study for the 345 index SNPs.
Two illustrative examples indicate how follow-up of WHRadjBMI associations from a very large study in a smaller study with specific fat depots quantified may prove useful. The top WHRadjBMI signal is located at an intronic RSPO3 locus (rs72959041; beta = −0.162; p = 2.1 × 10−293)—our work further clarifies that this signal is driven by an effect on VATadj (beta = −0.118; p = 7.8 × 10−13) and GFATadj (beta = 0.195; p = 3.2 × 10−32), but not ASATadj (beta = 0.029; p = 0.09). In contrast, a WHRadjBMI signal near LINC02029 (rs10049088; beta = 0.029; p = 1.5 × 10−59) is driven by ASATadj (beta = 0.054; p = 7.3 × 10−14) and GFATadj (beta = −0.034, p = 6.0 × 10−6), but has a VATadj-discordant signal (beta = −0.053, p = 8.7 × 10−13).
External validation
We pursued replication of our genome-wide significant loci with a prior meta-analysis of CT and MRI-derived VAT, ASAT, VAT adjusted for BMI (VATadjBMI), and VAT/ASAT ratio in up to 18,332 individuals27. Of the 76 SNP-trait associations across the traits of VAT, ASAT, VATadj, and VAT/ASAT ratio in this study, association results for 17 were available for comparison in published summary statistics27. Of these, 16 (94%) had directionally consistent effects (binomial test p = 2.7 × 10−4, Supplementary Data 12).
Transcriptome-wide association study
To prioritize genes, we conducted a transcriptome-wide association study (TWAS) using gene expression data from visceral and subcutaneous adipose tissue from GTEx v760. Across all traits, the most significant association was observed between GFATadj and CCDC92 (TWAS Z-score = 12.0; TWAS p = 2.7 × 10−33) in subcutaneous adipose tissue (Supplementary Data 13). The most significant eQTL for this association was shared with DNAH10OS (TWAS Z-score = 10.5; p = 8.2 × 10−26) and DNAH10 (TWAS Z-score = 7.9; p = 3.5 × 10−15). Prior work demonstrated that knockdown of CCDC92 or DNAH10 led to significant reduction of lipid accumulation in an adipocyte model19. Of note, predicted VATadj associations with CCDC92 and DNAH10 in visceral adipose tissue samples demonstrated the opposite direction of effect (CCDC92 Z-score = −6.7; p = 2.7 × 10−11; DNAH10 Z-score = −5.3; p = 1.1 × 10−7), suggesting fat depot discordant effects.
Another top TWAS signal was observed with GFATadj and IRS1 (Z-score = 9.1; p = 6.2 × 10−20) with the corresponding association with ASATadj having the same direction of effect (Z-score = 5.5; p = 4.6 × 10−8). Prior work has demonstrated that decreased IRS1 expression, the gene encoding the insulin receptor substrate, causes insulin resistance—our work further suggests that impaired expansion of the gluteofemoral and abdominal subcutaneous fat depots may be involved in this physiological insult47,61. Finally, a significant association was observed between VEGFB and GFATadj (Z-score = 7.0; p = 2.0 × 10−12), but not ASATadj (Z-score = 0.44, p = 0.66). Endothelial VEGFB is known to facilitate endothelial targeting of fatty acids to peripheral tissues and induce adipocyte thermogenesis, and transduction of VEGFB into mice improved metabolic health without changes in body weight62,63. These results suggest that maintenance of the gluteofemoral fat depot may partially explain the metabolic effects of VEGFB.
Tissue-specific enrichment analyses
We used stratified LD-score regression to probe for tissue-specific enrichment for each adiposity trait (Supplementary Data 14)64. A marked dichotomy was observed between the three raw fat depot volumes (VAT, ASAT, GFAT)—each highly genetically correlated with BMI—and the six derived local adiposity traits (VATadj, ASATadj, GFATadj, VAT/ASAT, VAT/GFAT, ASAT/GFAT). While VAT, ASAT, and GFAT showed a pattern of central nervous system (CNS) tissue enrichment—consistent with the enrichment pattern for BMI—local adiposity traits were characterized by adipose tissue signals with reduced CNS signals (Supplementary Figs. 16 and 17). These results further emphasize that the genetic basis of overall adiposity is driven largely by CNS processes—such as those governing appetite and satiety—whereas fat distribution is regulated at the level of the adipocyte and other peripheral tissues.
Rare variant association study
Up to 19,255 individuals with fat depots quantified and exome sequencing data available were included in rare variant association studies. We utilized two masks: one containing only predicted loss-of-function variants (pLoF) and a second combining pLoF with missense variants predicted to be deleterious by 5 out of 5 in silico prediction algorithms (pLoF + missense). We tested the association between the aggregated rare variant score with each mask and each inverse normal transformed phenotype using multivariable regression. Analyses were restricted to genes with at least ten variant carriers in the analyzed cohort, yielding up to 12,020 tested genes. Exome-wide significance was considered to be p < 0.05/12,020 = 4.2 × 10−6, while a Bonferroni-corrected study-wide significance threshold was set to p < 4.2 × 10−6/27 = 1.5 × 10−7. One exome-wide significant association was identified: pLoF + missense variants in PDE3B associated with increased GFATadj in females (24 carriers; beta = 0.98; p = 1.7 × 10−6) (Supplementary Data 15). Individuals who carry loss-of-function variants in PDE3B have previously been demonstrated to have reduced WHRadjBMI65. This study confirms and extends this result by demonstrating that females who carry pLoF + missense variants in PDE3B harbor increased GFATadj and reduced VATadj (beta = −0.70; p = 5.1 × 10−4)—consistent with a metabolically favorable fat distribution—and that these effects are attenuated in males (GFATadj beta = 0.08; p = 0.67; VATadj beta = −0.21; p = 0.27) (Fig. 5 and Supplementary Data 16).
A mask combining predicted loss-of-function variants and missense variants predicted to be deleterious by 5 out of 5 in silico prediction algorithms in PDE3B associated with GFATadj in females with exome-wide significance (Supplementary Data 15). Effect sizes with 95% confidence intervals are plotted for carrier status. Linear regressions were adjusted for age, age squared, imaging center, genotyping array, and the first ten principal components of genetic ancestry (Supplementary Data 16). Note that the carrier counts are with respect to individuals who had “adj” traits available. For the other six traits, the carrier counts are 26 carriers/9616 participants for males and 25 carriers/9879 participants for females.
Rare variant signals in two additional genes, while they did not reach our threshold for exome-wide significance, warrant discussion. pLoF + missense variants in PCSK1 associated with GFAT in sex-combined analysis (101 carriers; beta = 1.11; p = 7.5 × 10−6) and pLoF + missense variants in ACAT1 associated with VAT in females (23 carriers; beta = 2.66; p = 6.4 × 10−6). Both of these genes have previously been implicated in altering adiposity. Rare mutations in PCSK1 are known to cause monogenic obesity—here, a relatively symmetric pattern of increased GFAT, VAT (beta = 0.87; p = 4.1 × 10−4), and ASAT (beta = 1.04; p = 3.1 × 10−5) were observed in sex-combined analyses (Supplementary Data 16)66,67. In a study comparing obese women with or without type 2 diabetes, gene expression of ACAT1 was downregulated in the VAT and ASAT of obese women with type 2 diabetes and expression was restored after bariatric surgery and weight loss, suggesting a role in obesity-associated insulin resistance68.
Finally, we investigated if rare variants in known familial partial lipodystrophy genes PPARG and LMNA were associated with the adiposity traits defined in this study (Supplementary Data 17)8,10,69. The 17 carriers of a pLoF + missense variant in PPARG tended to have reduced GFATadj in sex-combined analysis (beta = −0.99, p = 0.05), consistent with a lipodystrophic-pattern of reduced peripheral adipose tissue deposition. We were unable to detect a significant association among the 51 carriers of rare LMNA variants, potentially related to inadequate statistical power or variant annotation.
Polygenic contribution to extremes of VATadj, ASATadj, and GFATadj
Because many individuals with lipodystrophy-like phenotypes—especially in its more subtle forms—do not harbor a known pathogenic rare variant, prior studies have begun to explore a potential “polygenic lipodystrophy,” in which an inherited component is instead driven by the cumulative impact of many common DNA variants10,19,20,70. In the context of the traits defined in this study, a lipodystrophy-like phenotype might be characterized by increased VATadj, decreased ASATadj, and/or decreased GFATadj. We set out to quantify the potential for genetic prediction of these traits by generating polygenic scores consisting of up to 1,125,301 variants for VATadj, ASATadj, and GFATadj traits using the LDpred2 algorithm71. To ensure no overlap between summary statistics and tested individuals, GWAS was conducted using a randomly selected 70% of participants. An additional 10% of participants was used as training data to select optimal LDpred2 hyperparameters and the remaining 20% of participants were held out for testing. In the test set, VATadj, ASATadj, and GFATadj polygenic scores explained 5.8%, 3.6%, and 7.0% of the corresponding trait variance, respectively (Supplementary Data 18 and 19). Participants at the tails of the distribution for any of the three local adiposity traits were enriched in extreme polygenic scores—for example, participants in the top 5% of the GFATadj distribution were nearly four times as likely to have a GFATadj polygenic score in the top 5% of the distribution (14.8% vs. 4.4%; OR = 3.81; 95% CI: 2.76–5.17) (Fig. 6 and Supplementary Fig. 18). Conversely, individuals with less than the 5th percentile of GFATadj were over three times as likely to have a GFATadj polygenic score less than the 5th percentile (14.3% vs. 4.7%; OR = 3.36; 95% CI: 2.32–4.77). These findings suggest that polygenic inheritance plays an important role in fat distribution, and that polygenic scores could feasibly be used to enrich cohorts for individuals with extreme imaging phenotypes.
For each fat depot “adj” trait, a polygenic score was trained using LDpred2 on 70% of the studied cohort and a 10% validation cohort was used to determine the optimal set of hyperparameters. Results in this figure correspond to the 20% imaged and testing set (N = 7795). Supplementary Fig. 18 shows the full distribution of each polygenic score in each tail of VATadj, ASATadj, and GFATadj.
We next tested the relationship between VATadj, ASATadj, and GFATadj polygenic scores and biomarkers of metabolic health (hemoglobin A1C, HDL cholesterol, serum triglycerides, and alanine aminotransferase (ALT)) and disease outcomes (type 2 diabetes, hypertension, and coronary artery disease) (Fig. 7 and Supplementary Data 20).
The central density plots indicate the distributions of VATadj, ASATadj, and GFATadj polygenic scores in genotyped individuals of the UK Biobank who were not imaged (N = 447,486). The dotted lines and shaded regions correspond to individuals in the top 5% and bottom 5% of the polygenic score. Forest plots to the right correspond to effect sizes of an indicator variable for being in the top 5% of the polygenic score (with identical color-coding to the density plots), while forest plots to the left correspond to effect sizes of an indicator variable for being in the bottom 5% of the polygenic score. Each polygenic score was residualized against the first ten principal components of genetic ancestry prior to being discretized, and each regression was adjusted for age at imaging, sex, and the first ten principal components of genetic ancestry. HbA1C hemoglobin A1C, HDL-c HDL-cholesterol, Trig triglycerides, ALT alanine aminotransferase, T2D prevalent type 2 diabetes (at time of imaging), CAD prevalent coronary artery disease, HTN prevalent hypertension. Corresponding data are found in Supplementary Data 20.
Within an independent dataset of 447,486 individuals of the UK Biobank who were genotyped, but not imaged, individuals in the top 5% of the GFATadj polygenic score had higher HDL-cholesterol (beta: 0.16 SD; 95% CI: 0.15–0.18; p = 8.2 × 10−107), lower serum triglycerides (beta: −0.16 SD; 95% CI: −0.18–−0.15; p = 1.9 × 10−120), lower serum ALT (beta: −0.09; 95% CI: −0.10–−0.07; p = 7.9 × 10−36), lower risk of type 2 diabetes (OR: 0.75; 95% CI: 0.70–0.79; p = 1.3 × 10−23), and lower risk of coronary artery disease (OR: 0.89; 95% CI: 0.85–0.93; p = 1.6 × 10−6). By contrast, those in the top 5% of the VATadj polygenic score tended to have increased risk of these disease outcomes with odds ratios for type 2 diabetes, coronary artery disease, and hypertension of 1.18, 1.12, and 1.09, respectively.
We aimed to externally validate associations with VATadj, ASATadj, and GFATadj polygenic scores in 7888 White participants of the Atherosclerosis Risk in Communities (ARIC) study72. Each polygenic score was associated with HDL-cholesterol, triglycerides, and type 2 diabetes in ARIC. Results were broadly consistent with the UK Biobank with the strongest associations observed with the GFATadj polygenic score—individuals in the top 10% of the GFATadj polygenic score had higher HDL-cholesterol (beta: 0.14 SD, 95% CI: 0.07–0.22, p = 1.5 × 10−4), lower serum triglycerides (beta: −0.16 SD; 95% CI: −0.23–−0.08, p = 3.2 × 10−5), and lower risk of prevalent type 2 diabetes (OR: 0.57; 95% CI: 0.41–0.78, p = 5.5 × 10−4) (Supplementary Data 21).
Discussion
In this study, we investigated the inherited basis of body fat distribution using VAT, ASAT, and GFAT volumes quantified from body MRI in up to 38,965 individuals. Local adiposity traits derived from these fat depots had a significant inherited component, enabling identification of 250 unique loci across all traits. The increased precision afforded by image-derived quantification confirmed and extended prior work indicating significant sex-dimorphism, refined depot-specific associations for loci previously identified for WHRadjBMI, and led to the discovery of newly-associated loci, including a missense variant in SERPINA1 that predisposes to a metabolically healthier fat distribution. Polygenic scores for local adiposity traits were highly enriched among those with “lipodystrophy-like” fat distributions and were associated with cardiometabolic traits in a depot-specific fashion. These results have at least four implications.
First, traits aiming to quantify variation in body habitus—even when they are image-derived measurements of specific fat depot volumes as in this study—tend to be highly observationally and genetically correlated with one another and with BMI. GWAS of raw VAT, ASAT, and GFAT volumes each identified a well-known intronic FTO variant—characteristic of BMI—as a top signal, and cell-enrichment analyses of each unadjusted fat depot displayed a pattern of CNS cell-enrichment, consistent with the signal for BMI64. By contrast, fat depot volumes adjusted-for-BMI-and-height and fat depot ratios—traits that capture local adiposity—were more heritable than measures of overall adiposity, revealed depot-specific genetic architecture, and displayed a pattern of adipose tissue cell-enrichment. As large cohorts with body imaging become more prominent, careful consideration of this correlation structure is warranted to enable interpretation of genetic association results. For example, a measurement of VAT predicted from a model using primarily anthropometric traits was very highly genetically correlated with BMI (rg = 0.93), suggesting that the resultant genetic associations may predominantly reflect a component of VAT that is complementary to VATadj (rg with BMI = −0.16) in this study29. Additional investigation of how best to utilize composite phenotypes that jointly represent several correlated adiposity traits may prove useful73,74.
Second, GFAT is highly heritable (GFATadj h2 = 0.41)—particularly in females (GFATadj h2 = 0.52)—with a genetic architecture that is distinct from VAT and ASAT when adjusted for overall adiposity. Most prior genetic studies of imaging-derived adiposity traits to date have been limited to VAT and ASAT—in this study, only 13 of 54 genome-wide significant loci for GFATadj overlapped with either VATadj or ASATadj26,27,28. Individuals with a GFATadj polygenic score in the bottom 5% were enriched for adverse cardiometabolic biomarker profiles and increased risk of type 2 diabetes and coronary artery disease. These observations lend further support to the hypothesis that a primary insult in a metabolically unhealthy fat distribution is the inability of the gluteofemoral fat depot to adequately expand4,75. Additional study of GFAT depots—or related measures such as gynoid fat from DEXA scans—in future biobank-scale studies is warranted to determine the consistency of these genetic associations across diverse age and ancestry groups.
Third, this study extends prior work suggesting that common genetic variation—as captured by a polygenic score—contributes to extreme fat distribution phenotypes10,19,20,70. While several of the familial partial lipodystrophies (FPLD) are known to be caused by monogenic variation in genes like LMNA and PPARG, FPLD type 1 has not been linked to a single mutation, leading some to suggest that this disease may be polygenic in nature10. Lotta et al. provided evidence for this by demonstrating that individuals with FPLD1 had a higher burden of a 53-SNP insulin resistance polygenic score compared to the general population19. In this study, individuals who harbor lower than average GFATadj or ASATadj and/or higher than average VATadj tended to manifest a mild lipodystrophy-like phenotype. We demonstrate that individuals at the extremes of these local adiposity traits are enriched in extreme polygenic scores suggesting that polygenic scores may be helpful in identifying this subgroup of individuals for future focused investigations. For example, growth hormone releasing hormone analogs—such as tesamorelin—have previously been shown to lead to a selective reduction of VAT in patients with obesity or HIV-associated lipodystrophy76,77. Whether a local adiposity polygenic score—perhaps in combination with emerging imaging tools for identifying lipodystrophies—could identify a subset of individuals with obesity and polygenic lipodystrophy who may benefit from these fat redistribution agents in addition to traditional obesity therapy is an area for future investigation78.
Fourth, these results lay the scientific foundation for variant-to-function studies to link fat distribution-associated genetic risk loci to effector genes and mechanisms of action in depot-specific adipocyte model systems79. Such targeted perturbation studies in subcutaneous and visceral adipocyte cell lines may reveal key biological pathways driving fat distribution, and may generate therapeutic hypotheses for adverse fat distribution-related traits19,80.
In conclusion, we carried out genetic association studies of local adiposity traits in a large cohort of individuals with MRI imaging. Our work characterizes the depot-specific genetic architecture of visceral, abdominal subcutaneous, and gluteofemoral adipose tissue, and extends efforts to define and identify individuals with polygenic lipodystrophy.
Methods
Study population
The UK Biobank is an observational study that enrolled over 500,000 individuals between the ages of 40 and 69 years between 2006 and 2010, of whom 43,521 underwent MRI imaging between 2014 and 202081,82. Our group previously estimated VAT, ASAT, and GFAT volumes in 40,032 individuals of the imaged cohort after excluding 3489 (8.0%) scans based on technical problems or artifacts5. A subset of 39,076 individuals with genotype array data available was studied here. Compared to non-imaged individuals of the UK Biobank at enrollment, imaged individuals were younger (mean age 56 years vs. 57 years), less likely to be female (51% vs. 55%), and more likely to be of white British ancestry (87% vs. 84%) (Supplementary Data 2). Individuals were not excluded on the basis of ancestry. This analysis of data from the UK Biobank was approved by the Mass General Brigham institutional review board and was performed under UK Biobank application #7089.
Deriving local adiposity traits
The focus of this study was to investigate the genetic architecture of fat distribution independent of the overall size of an individual. Two sets of traits were derived for this purpose: “adj” traits and fat depot ratios. “adj” traits represent residuals of the fat depot in question in sex-specific linear regressions against age, age squared, BMI, and height. We provide justification in the Supplementary Methods for adjusting for both BMI and height as opposed to only BMI. In brief, adjusting only for BMI introduces a significant genetic correlation of each adj trait with height (most pronounced with ASAT and GFAT). Several prior studies have suggested that adjusting for heritable covariates can lead to spurious genetic associations due to collider bias83,84. We investigated the extent to which VATadj, ASATadj, and GFATadj loci may be driven by collider bias with BMI or height and found little evidence for collider bias making a significant contribution to these results (Supplementary Methods and Supplementary Data 22).
Genotyping, imputation, and QC
Genotyping in the UK Biobank was done with two custom genotyping arrays: UK BiLEVE and Axiom85. Imputation was done using the UK10K and 1000 Genomes Phase 3 reference panels86,87. Prior to analysis, genotyped SNPs were filtered based on the following criteria, only including variants if: (1) MAF ≥ 1%, (2) Hardy-Weinberg equilibrium (HWE) p > 1 × 10−15, (3) genotyping rate ≥ 99%, and (4) LD pruning using R2 threshold of 0.9 with window size of 1000 markers and step size of 100 marker88,89. This process resulted in 433,616 SNPs available for genetic relationship matrix (GRM) construction. Imputed SNPs with MAF < 0.005 or imputation quality (INFO) score <0.3 were excluded. Note that the MAF filter was applied to the UK Biobank imputed file prior to subsetting to the imaged substudy. These criteria resulted in a total of 11,485,690 imputed variants available for analysis.
Participant were excluded from analysis if they met any of the following criteria: (1) mismatch between self-reported sex and sex chromosome count, (2) sex chromosome aneuploidy, (3) genotyping call rate <0.95, or (4) were outliers for heterozygosity. Up to 38,965 participants were available for analysis (37,641 for adj traits because these individuals also had to have BMI and height available).
Common variant association studies
Nine traits were analyzed (VAT, ASAT, GFAT, VATadj, ASATadj, GFATadj, VAT/ASAT, VAT/GFAT, and ASAT/GFAT) in three contexts (sex-combined, male only, female only), leading to 27 analyses in total. SNP-heritability was estimated using BOLT-REML v2.3.490,91. Genetic correlations between traits were estimated using cross-trait LD-score regression (ldsc v1.0.1) using default settings33,34.
Prior to conducting GWAS, each trait was inverse-normal transformed. Each analysis was adjusted for age at the time of MRI, age squared, sex (except in sex-stratified analyses), the first ten principal components of genetic ancestry, genotyping array, and MRI imaging center. BOLT-LMM v2.3.4 was used to carry out GWAS accounting for cryptic population structure and sample relatedness90,91. After the QC protocol detailed above, 433,616 SNPs were available for GRM construction. A threshold of p < 5 × 10−8 was used to denote genome-wide significance, while a threshold of p < 5 × 10−8/27 = 1.9 × 10−9 was used to denote study-wide significance.
Lead SNPs were prioritized with LD clumping. LD clumping was done with the -clump function in PLINK to isolate independent signals for each GWAS. The parameters were as follows: -clump-p1 5E−08, -clump-p2 5E−06, -clump-r2 0.1, -clump-kb 1000, which can be interpreted as follows: variants with p < 5E−08 are chosen starting with the lowest p value, and for each variant chosen, all other variants with p < 5E−06 within a 1000 kb region and r2 > 0.1 with the index variant are assigned to that index variant. This process is repeated until all variants with p < 5E−08 are assigned an LD clump. An LD reference panel for this task was constructed using a random sample of 3000 individuals from the studied.
The extent of genomic inflation vs. polygenicity was assessed by computing the LD-score regression intercept (ldsc v1.0.1) using default settings33.
A lead SNP was defined as newly-identified if it was not in LD (R2 < 0.1) with any SNP in the GWAS catalog (downloaded June 08, 2021) with genome-wide significant association (p < 5 × 10−8) with any “DISEASE/TRAIT” containing the following characters: (1) “body mass”, (2) “BMI”, (3) “adipos”, (4) “fat”, (5) “waist”, (6) “hip circ”, or (7) “whr”. These characters captured key anthropometric traits of interest (e.g., BMI, waist circumference, hip circumference, waist-to-hip ratio) as well as other related traits of interest (e.g., VAT, predicted VAT, fat impedance measures).
Clustering to classify gluteofemoral adiposity signals
Clustering analysis was performed for GFATadj and GFAT association signals. We started with all 250 lead SNPs significantly associated with any of the nine adiposity traits and extracted those associated with the primary trait (e.g., GFATadj) with nominal significance (p < 0.05) for each analysis. To ensure that only independent signals were used for the clustering, variants were LD-pruned using a LD threshold of r2 = 0.1. When two SNPs were found to be in LD above this threshold, the variant with the lower p value was retained.
Summary statistics were gathered from GWAS performed in the UK Biobank for 32 cardiometabolic traits (Supplementary Data 6). For each trait GWAS, the regression coefficient betas was divided by the SE to obtain standardized effect sizes. These standardized effects were further scaled by dividing by the square root of the variant’s sample size for the given trait GWAS and then multiplying by the square root of the median sample size of all GWAS. Since all summary statistics were sourced from UK Biobank, this additional scaling had a negligible effect.
The clustering traits were then filtered to retain those relevant to the analysis by removing any that were not associated with at least one variant at a Bonferroni p value threshold (0.05/number of SNPs). When two traits had highly correlated Z-scores (|r| > 0.85), the trait with the lower minimum p value was kept and the other removed. The remaining standardized effect sizes made up the variant-trait association matrix, Z (N variants by M traits).
In order to satisfy the non-negative requirement of Bayesian non-negative matrix factorization (bNMF), each column was split into two arrays: one with the positive Z-scores and the other with the absolute value of the negative Z-scores. This means that the final association matrix, X, contained N variants by 2M traits.
The bNMF clustering was performed as previously described20. The procedure attempts to approximate the association matrix by factorizing X into two matrices, W (2M by K) and HT (N by K), with an optimal rank K. bNMF is designed to suggest an optimal K best explaining X at the balance between an error measure, ||X − WH|2, and a penalty for model complexity derived from a non-negative half-normal prior for W and H. In addition, bNMF exploits an automatic relevance determination technique to iteratively regress out irrelevant components in explaining the observed data X. The exact objective function optimized by bNMF is a posterior, which has two opposing contributions from the likelihood (Frobenius norm) and the regularization penalty (L2-norm of W and H coupled by the relevance weights). For all analyses, bNMF was run with 100 iterations for each. All analyses converged in ≥92% of iterations to their given K solution. Code used in the bNMF clustering is available on GitHub: https://github.com/kwesterman/bnmf-clustering.
Identification of sex-dimorphic signals
Genetic correlations between sexes for each of the adiposity traits were computed using cross-trait LD-score regression as described above.
Using sex-specific GWAS summary statistics for each of the six local adiposity traits (VATadj, ASATadj, GFATadj, VAT/ASAT, VAT/GFAT, ASAT/GFAT), we tested each of the 220 genetic loci that were genome-wide significant for any of the six local adiposity traits in either sex-combined or sex-stratified analyses for sex dimorphism by computing the t-statistic:
where beta is the effect size for an adiposity trait in sex-stratified GWAS, se is the standard error, and r is the genome-wide Spearman rank correlation coefficient between males and females. The t-statistic and associated p value (pdiff) were computed using the EasyStrata software92. Given that 220 independent loci were tested, a significance threshold of pdiff < 0.05/220 = 2.3 × 10−4 was used.
WHRadjBMI loci lookups
A recent meta-analysis for the WHRadjBMI trait across 694,649 individuals revealed 346 unique associated loci12. Of these 346 loci, the primary signals for 345 loci were among the imputed variants available for analysis in this study. We plotted the effect sizes for VATadj, ASATadj, and GFATadj for each of these 345 loci and further quantified the frequency of “WHRadjBMI-discordance” defined as either (1) WHRadjBMI and VATadj effects going in opposite directions, (2) WHRadjBMI and ASATadj effects going in opposite directions, or (3) WHRadjBMI and GFATadj effects going in the same direction. For each adiposity trait in the “WHRadjBMI-discordance” analysis, we excluded loci for which the effect size beta was smaller than the SE to avoid inflating the fraction of “WHRadjBMI-discordant” loci.
External validation with prior meta-analysis
External validation for 76 genome-wide significant SNP-trait associations with VAT, ASAT, VATadj, and VAT/ASAT ratio was pursued using summary statistics downloaded from the GWAS catalog of a multiethnic genome-wide meta-analysis of ectopic fat depots in up to 2.6 million SNPs in up to 18,332 individuals27,35. Alleles were aligned and the z-score for each SNP from the previous study were compared with the effect sizes in the current study to determine concordance.
Transcriptome-wide association study
For each of the six local adiposity traits (VATadj, ASATadj, GFATadj, VAT/ASAT, VAT/GFAT, ASAT/GFAT), we performed a TWAS to prioritize genes on the basis of imputed cis-regulated gene expression using FUSION with default settings60,93,94. Pre-computed gene expression weights from GTEx v7 were used as downloaded from the FUSION website (http://gusevlab.org/projects/fusion/)60. Reference weights for visceral adipose tissue were used for VATadj, while those for subcutaneous adipose tissue were used for ASATadj, GFATadj, and ASAT/GFAT ratio. Weights from both visceral and subcutaneous adipose tissue were used for VAT/ASAT and VAT/GFAT ratios.
Cell- and tissue-specific enrichment
We used stratified LD-score regression to identify cell types that are most relevant for each of the nine adiposity traits (VAT, ASAT, GFAT, VATadj, ASATadj, GFATadj, VAT/ASAT, VAT/GFAT, and ASAT/GFAT) and BMI64. We carried out this analysis using ldsc v1.0.1 with default settings and using two gene expression datasets that are described in the manuscript outlining stratified LD-score regression64: GTEx95 and the “Franke lab”96,97 dataset.
Sequencing and sample quality control for rare-variant association study
We conducted rare-variant association studies using data from the 200,643 exomes released by the UK Biobank98. Whole-exome sequencing was performed by the Regeneron Genetics Center using an updated Functional Equivalence protocol that retains original quality scores in the CRAM files (referred to as the OQFE protocol) as previously described98. The DTxGen Exome Research Panel v1.0 including supplemental probes was used for exome capture for this dataset (https://biobank.ctsu.ox.ac.uk/showcase/label.cgi?id=170). In total, 19,396 genes in the targets of 38Mbp were covered. In total, 75 × 75 bp paired-end reads were sequenced on the Illumina NovaSeq 6000 platform. For each sample in the targeted region, more than 95.2% of sites were covered by more than 20 reads. We downloaded the pVCF file provided by the UK Biobank, and then applied additional genotype call, variant, and sample quality control99.
The individual genotype call was set as missing if reads depth (DP) ≤ 10 or DP ≥ 200, if homozygous reference allele with genotype quality (GQ) ≤ 20 or the ratio of alt allele reads over all of the covered reads >0.1, if heterozygous with the ratio of alt allele reads over all of the covered reads <0.2 or Phred-scaled likelihood (PL) of the reference allele <20, or if homozygous alternate with the ratio of alt allele reads over all of the covered reads <0.9 or PL of reference allele <20. The variant quality control was performed using the following exclusion criteria:
-
Variants in low-complexity regions of the genome that preclude accurate read alignment as previously defined100.
-
Variants in segmental duplication region of the genome100,101.
-
Hardy-Weinberg disequilibrium (HWE) p value <1 × 10−15.
-
Variant call rate <90%.
-
Monomorphic sites after the above genotype call quality control.
After the above genotype call and variant QC, we selected a subset of high-quality variants for inferring the genetic kinship matrix and genetic sex used for sample QC. We selected independent autosome variants by MAF > 0.1%, missingness <1%, and HWE p > 10−6. We further pruned the variants using PLINK2 software102 with a window size of 200, step size 100, and R2 = 0.1 and removed indels and strand ambiguous SNPs. Based on these variants, we used KING (version 2.2.5)103 to infer the genetic kinship matrix. We further selected X-chromosomal variants, not within the pseudo-autosomal regions, based on the sample variant QC criteria as for the autosome variants and did the same variant pruning procedure. We then inferred the genetic sex based on the F statistics by PLINK2 software, F > 0.8 was set to male, while samples with F < 0.5 were set to female. Eighty samples were removed because of the discordance of genetic sex with self-reported sex. We further removed samples if:
-
The ratio of heterozygote/homozygote beyond 8 standard deviations (N = 100 samples removed).
-
The ratio of the number of SNVs/indels beyond 8 standard deviations (N = 1 samples removed).
-
The number of singletons was beyond 8 standard deviations (N = 111 samples removed).
-
Genotype call rate <90% (N = 1 sample removed).
-
Withdrawal of informed consent (N = 13 samples removed).
We further randomly removed one sample if a pair of samples had second-degree relative or closer kinship, defined as kinship coefficient >0.088474 (N = 1563 samples removed). Of all the above QC passed samples, 19,255 samples out of the 40,032 having image-derived traits were used in the downstream rare variant burden test. We converted the genetic coordinates from GRCh38 to GRCh37 using CrossMap software (version: v0.3.3)104.
Approach to variant annotation and weighting
To identify rare (MAF <0.1%) high-confidence predicted inactivating variants, we applied the previously validated Loss-Of-Function Transcript Effect Estimator (LOFTEE) algorithm implemented within the Ensembl Variant Effect Predictor (VEP) software program as a plugin, VEP version 96.0105,106. The LOFTEE algorithm identifies stop-gain, splice-site disrupting, and frameshift variants. The algorithm includes a series of flags for each variant class that collectively represent “low-confidence” inactivating variants. In this study, we studied only variants that were “high-confidence” inactivating variants without any flag values. This aggregation strategy will be referred to hereafter as putative loss-of-function (“pLoF“).
To identify rare (MAF <0.1%) predicted damaging missense variants, we included variants predicted to be damaging by all of five computational prediction algorithms107,108,109. In brief, predictions were retrieved from the dbNSFP database110, version 2.9.3, with the most severe prediction across multiple transcripts used. We focused on five prediction algorithms: SIFT111 (including variants annotated as damaging), PolyPhen2-HDIV and PolyPhen2-HVAR112 (including variants annotated as possibly or probably damaging), LRT113 (including variants annotated as deleterious), and MutationTaster114 (including variants annotated as disease-causing-automatic or disease-causing). Within the association testing framework, this class of variants was given a gene-specific weight based on the relative cumulative frequency of these predicted damaging missense variants as compared to the cumulative frequency of high-confidence predicted inactivating variants identified by LOFTEE algorithm using a previously recommended approach:115,116 given the cumulative allele frequency of all of the LOFTEE high-confidence rare variants of a gene (G) as fL, the cumulative allele frequency of all of the predicted damaging missense variants as fM, the weight for the missense variants was estimated as the quantity in Eq. (2) and capped at 1.0:
For genes without LOFTEE high-confidence rare variants, the weight for missense variants is 1.0. This aggregation strategy will be referred to hereafter as putative loss-of-function plus missense (“pLoF + missense”).
Statistical analysis
We tested the association between the aggregated rare variant score (the weighted sum of the qualified variant of each gene) and each inverse normal transformed phenotype using a multivariable regression model in sex-combined and sex-stratified models. Analyses were restricted to genes that had at least ten variant carriers in the analyzed cohort. An individual’s gene-specific score was computed according to the weighting strategy described above and capped at one. The covariates were the same as the common variant association test. Given the filter of ten variant carriers, sex-combined analyses tested 12,020 genes and so a gene was recognized as exome-wide significant if the gene’s p value was smaller than the Bonferroni-corrected p value threshold of 0.05/12,020 = 4.2 × 10−6.
Polygenic score
We used the LDpred2 algorithm71 to derive genome-wide polygenic scores for each trait. We randomly selected 350,000 White British ancestry individuals from the UK Biobank to use as the LD reference panel85, and used HapMap3 variants with MAF > 0.5% in the LD reference panel to compute the LD correlation matrix. For each trait, we partitioned the samples into three independent portions: 70% to run the GWAS for making the summary statistics, 10% to select the optimal hyperparameters, and 20% to test performance. We randomly removed one sample in a pair if the pair had a genetic relationship closer than a second-degree genetic relationship in the last two partitions of samples, and checked the pairwise relationship across the whole dataset. For the hyperparameters of the LDpred2 algorithm, we grid searched three parameters: (1) 0.7, 1, and 1.4 times of genome-wide heritability estimation, (2) whether or not to use a sparse LD correlation matrix, and (3) 17 different estimates of the proportion of causal variants selecting from [0.18,0.32,0.56,1] × 10[0,−1,−2,−3] and 0.0001. In total, we tested 3 × 2 × 17 = 102 grid points.
For all downstream analyses, each polygenic score was residualized against the first ten principal components of genetic ancestry prior to regression with the dependent variable of interest, and each regression was adjusted for age at the time of imaging, sex, and the first ten principal components of genetic ancestry.
Polygenic score external validation in ARIC
The ARIC study is a prospective cohort study that—beginning in 1987—enrolled white and black participants between the ages of 45 and 64 years72. Genotype and clinical data were retrieved from the National Center for Biotechnology Information dbGAP server (accession number phg000035.v1). VATadj, ASATadj, and GFATadj polygenic scores were computed using identical LDpred2 weights and the optimal hyperparameter set for UK Biobank analyses. Circulating biomarkers and clinical risk factor ascertainment was performed at time of enrollment as previously described72.
Reporting summary
Further information on research design is available in the Nature Research Reporting Summary linked to this article.
Data availability
This research has been conducted using the UK Biobank Resource under Application Number #7089. The raw UK Biobank data are made available to researchers from universities and other research institutions with genuine research inquiries, following IRB and UK Biobank approval. The GWAS summary statistics and polygenic score weights generated in this study will be made available for download from the Cardiovascular Disease Knowledge Portal under the “Downloads” tab at https://cvd.hugeamp.org/ at the time of publication. All other relevant results are available in the Supplementary Data.
References
González-Muniesa, P. et al. Obesity. Nat. Rev. Dis. Prim. 3, 1–18 (2017).
Kivimäki, M. et al. Overweight, obesity, and risk of cardiometabolic multimorbidity: pooled analysis of individual-level data for 120 813 adults from 16 cohort studies from the USA and Europe. Lancet Public Health 2, e277–e285 (2017).
Stefan, N., Schick, F. & Häring, H.-U. Causes, characteristics, and consequences of metabolically unhealthy normal weight in humans. Cell Metab. 26, 292–300 (2017).
Stefan, N. Causes, consequences, and treatment of metabolically unhealthy fat distribution. Lancet Diabetes Endocrinol. 8, 616–627 (2020).
Agrawal, S. et al. Association of machine learning-derived measures of body fat distribution in >40,000 individuals with cardiometabolic diseases. medRxiv. https://doi.org/10.1101/2021.05.07.21256854 (2021).
Agarwal, A. K. & Garg, A. A novel heterozygous mutation in peroxisome proliferator-activated receptor-γ gene in a patient with familial partial lipodystrophy. J. Clin. Endocrinol. Metab. 87, 408–408 (2002).
Agostini, M. et al. Non-DNA binding, dominant-negative, human PPARgamma mutations cause lipodystrophic insulin resistance. Cell Metab. 4, 303–311 (2006).
Shackleton, S. et al. LMNA, encoding lamin A/C, is mutated in partial lipodystrophy. Nat. Genet. 24, 153–156 (2000).
Ajluni, N. et al. Spectrum of disease associated with partial lipodystrophy: lessons from a trial cohort. Clin. Endocrinol. 86, 698–707 (2017).
Lim, K., Haider, A., Adams, C., Sleigh, A. & Savage, D. B. Lipodistrophy: a paradigm for understanding the consequences of ‘overloading’ adipose tissue. Physiol. Rev. 101, 907–993 (2021).
Shungin, D. et al. New genetic loci link adipose and insulin biology to body fat distribution. Nature 518, 187–196 (2015).
Pulit, S. L. et al. Meta-analysis of genome-wide association studies for body fat distribution in 694 649 individuals of European ancestry. Hum. Mol. Genet. 28, 166–174 (2019).
Rask-Andersen, M., Karlsson, T., Ek, W. E. & Johansson, Å. Genome-wide association study of body fat distribution identifies adiposity loci and sex-specific genetic effects. Nat. Commun. 10, 339 (2019).
Pietiläinen, K. H. et al. Agreement of bioelectrical impedance with dual-energy X-ray absorptiometry and MRI to estimate changes in body fat, skeletal muscle and visceral fat during a 12-month weight loss intervention. Br. J. Nutr. 109, 1910–1916 (2013).
Ling, C. H. Y. et al. Accuracy of direct segmental multi-frequency bioimpedance analysis in the assessment of total body and segmental body composition in middle-aged adult population. Clin. Nutr. Edinb. Scotl. 30, 610–615 (2011).
Emdin, C. A. et al. Genetic association of waist-to-hip ratio with cardiometabolic traits, type 2 diabetes, and coronary heart disease. JAMA 317, 626–634 (2017).
Lotta, L. A. et al. Association of genetic variants related to gluteofemoral vs abdominal fat distribution with type 2 diabetes, coronary disease, and cardiovascular risk factors. JAMA 320, 2553–2563 (2018).
Yaghootkar, H. et al. Genetic evidence for a link between favorable adiposity and lower risk of type 2 diabetes, hypertension, and heart disease. Diabetes 65, 2448–2460 (2016).
Lotta, L. A. et al. Integrative genomic analysis implicates limited peripheral adipose storage capacity in the pathogenesis of human insulin resistance. Nat. Genet. 49, 17–26 (2017).
Udler, M. S. et al. Type 2 diabetes genetic loci informed by multi-trait associations point to disease mechanisms and subtypes: a soft clustering analysis. PLoS Med. 15, e1002654 (2018).
Ji, Y. et al. Genome-wide and abdominal MRI data provide evidence that a genetically determined favorable adiposity phenotype is characterized by lower ectopic liver fat and lower risk of type 2 diabetes, heart disease, and hypertension. Diabetes 68, 207–219 (2019).
Martin, S. et al. Genetic evidence for different adiposity phenotypes and their opposing influence on ectopic fat and risk of cardiometabolic disease. Diabetes. https://doi.org/10.2337/db21-0129 (2021).
Heald, A. H. et al. Genetically defined favourable adiposity is not associated with a clinically meaningful difference in clinical course in people with type 2 diabetes but does associate with a favourable metabolic profile. Diabet. Med. J. Br. Diabet. Assoc. 38, e14531 (2021).
Wilman, H. R. et al. Genetic studies of abdominal MRI data identify genes regulating hepcidin as major determinants of liver iron concentration. J. Hepatol. 71, 594–602 (2019).
Haas, M. E. et al. Machine learning enables new insights into clinical significance of and genetic contributions to liver fat accumulation. medRxiv https://doi.org/10.1101/2020.09.03.20187195 (2020).
Fox, C. S. et al. Genome-wide association for abdominal subcutaneous and visceral adipose reveals a novel locus for visceral fat in women. PLoS Genet. 8, e1002695 (2012).
Chu, A. Y. et al. Multiethnic genome-wide meta-analysis of ectopic fat depots identifies loci associated with adipocyte development and differentiation. Nat. Genet. 49, 125–130 (2017).
Liu, Y. et al. Genetic architecture of 11 organ traits derived from abdominal MRI using deep learning. eLife 10, e65554 (2021).
Karlsson, T. et al. Contribution of genetics to visceral adiposity and its relation to cardiovascular and metabolic disease. Nat. Med. 25, 1390–1395 (2019).
Chen, G.-C. et al. Association between regional body fat and cardiovascular disease risk among postmenopausal women with normal body mass index. Eur. Heart J. 40, 2849–2855 (2019).
Pou, K. M. et al. Patterns of abdominal fat distribution: the Framingham Heart Study. Diabetes Care 32, 481–485 (2009).
Hiuge-Shimizu, A. et al. Absolute value of visceral fat area measured on computed tomography scans and obesity-related cardiovascular risk factors in large-scale Japanese general population (the VACATION-J study). Ann. Med. 44, 82–92 (2012).
Bulik-Sullivan, B. K. et al. LD score regression distinguishes confounding from polygenicity in genome-wide association studies. Nat. Genet. 47, 291–295 (2015).
Bulik-Sullivan, B. et al. An atlas of genetic correlations across human diseases and traits. Nat. Genet. 47, 1236–1241 (2015).
Buniello, A. et al. The NHGRI-EBI GWAS Catalog of published genome-wide association studies, targeted arrays and summary statistics 2019. Nucleic Acids Res. 47, D1005–D1012 (2019).
Bradfield, J. P. et al. A trans-ancestral meta-analysis of genome-wide association studies reveals loci associated with childhood obesity. Hum. Mol. Genet. 28, 3327–3338 (2019).
Frayling, T. M. et al. A common variant in the FTO gene is associated with body mass index and predisposes to childhood and adult obesity. Science 316, 889–894 (2007).
Locke, A. E. et al. Genetic studies of body mass index yield new insights for obesity biology. Nature 518, 197–206 (2015).
Sinnott-Armstrong, N. et al. Genetics of 35 blood and urine biomarkers in the UK Biobank. Nat. Genet. 53, 185–194 (2021).
Zhu, Z. et al. Shared genetic and experimental links between obesity-related traits and asthma subtypes in UK Biobank. J. Allergy Clin. Immunol. 145, 537–549 (2020).
Mahajan, A. et al. Fine-mapping type 2 diabetes loci to single-variant resolution using high-density imputation and islet-specific epigenome maps. Nat. Genet. 50, 1505–1513 (2018).
Mullin, B. H. et al. Identification of a role for the ARHGEF3 gene in postmenopausal osteoporosis. Am. J. Hum. Genet. 82, 1262–1269 (2008).
You, J.-S. et al. ARHGEF3 regulates skeletal muscle regeneration and strength through autophagy. Cell Rep. 34, 108594 (2021).
Diabetes Genetics Initiative of Broad Institute of Harvard and MIT, Lund University, and Novartis Institutes of BioMedical Research. et al. Genome-wide association analysis identifies loci for type 2 diabetes and triglyceride levels. Science 316, 1331–1336 (2007).
Zeggini, E. et al. Replication of genome-wide association signals in UK samples reveals risk loci for type 2 diabetes. Science 316, 1336–1341 (2007).
Scott, L. J. et al. A genome-wide association study of type 2 diabetes in Finns detects multiple susceptibility variants. Science 316, 1341–1345 (2007).
Chen, Z. et al. Functional screening of candidate causal genes for insulin resistance in human preadipocytes and adipocytes. Circ. Res. 126, 330–346 (2020).
Nono Nankam, P. A. et al. Distinct abdominal and gluteal adipose tissue transcriptome signatures are altered by exercise training in African women with obesity. Sci. Rep. 10, 10240 (2020).
Loh, N. Y. et al. RSPO3 impacts body fat distribution and regulates adipose cell biology in vitro. Nat. Commun. 11, 2797 (2020).
Loos, R. J. F. & Kilpeläinen, T. O. Genes that make you fat, but keep you healthy. J. Intern. Med. 284, 450–463 (2018).
Emdin, C. A. et al. DNA sequence variation in ACVR1C encoding the activin receptor-like kinase 7 influences body fat distribution and protects against type 2 diabetes. Diabetes 68, 226–234 (2019).
Zorzetto, M. et al. SERPINA1 gene variants in individuals from the general population with reduced α1-antitrypsin concentrations. Clin. Chem. 54, 1331–1338 (2008).
van der Harst, P. & Verweij, N. Identification of 64 novel genetic loci provides an expanded view on the genetic architecture of coronary artery disease. Circ. Res. 122, 433–443 (2018).
Justice, A. E. et al. Protein-coding variants implicate novel genes related to lipid homeostasis contributing to body-fat distribution. Nat. Genet. 51, 452–469 (2019).
Lumish, H. S., O’Reilly, M. & Reilly, M. P. Sex differences in genomic drivers of adipose distribution and related cardiometabolic disorders: opportunities for precision medicine. Arterioscler. Thromb. Vasc. Biol. 40, 45–60 (2020).
Pettersson, A. M. L. et al. MAFB as a novel regulator of human adipose tissue inflammation. Diabetologia 58, 2115–2123 (2015).
Emdin, C. A. et al. Association of genetic variation with cirrhosis: a multi-trait genome-wide association and gene-environment interaction study. Gastroenterology 160, 1620–1633.e13 (2021).
Hua, X. et al. Non-alcoholic fatty liver disease is an influencing factor for the association of SHBG with metabolic syndrome in diabetes patients. Sci. Rep. 7, 14532 (2017).
Randall, J. C. et al. Sex-stratified genome-wide association studies including 270,000 individuals show sexual dimorphism in genetic loci for anthropometric traits. PLoS Genet. 9, e1003500 (2013).
Gusev, A. et al. Integrative approaches for large-scale transcriptome-wide association studies. Nat. Genet. 48, 245–252 (2016).
Kilpeläinen, T. O. et al. Genetic variation near IRS1 associates with reduced adiposity and an impaired metabolic profile. Nat. Genet. 43, 753–760 (2011).
Hagberg, C. E. et al. Vascular endothelial growth factor B controls endothelial fatty acid uptake. Nature 464, 917–921 (2010).
Robciuc, M. R. et al. VEGFB/VEGFR1-induced expansion of adipose vasculature counteracts obesity and related metabolic complications. Cell Metab. 23, 712–724 (2016).
Finucane, H. K. et al. Heritability enrichment of specifically expressed genes identifies disease-relevant tissues and cell types. Nat. Genet. 50, 621–629 (2018).
Emdin, C. A. et al. Analysis of predicted loss-of-function variants in UK Biobank identifies variants protective for disease. Nat. Commun. 9, 1613 (2018).
Jackson, R. S. et al. Obesity and impaired prohormone processing associated with mutations in the human prohormone convertase 1 gene. Nat. Genet. 16, 303–306 (1997).
Akbari, P. et al. Sequencing of 640,000 exomes identifies GPR75 variants associated with protection from obesity. Science 373, eabf8683 (2021).
Dharuri, H. et al. Downregulation of the acetyl-CoA metabolic network in adipose tissue of obese diabetic individuals and recovery after weight loss. Diabetologia 57, 2384–2392 (2014).
Hegele, R. A., Cao, H., Frankowski, C., Mathews, S. T. & Leff, T. PPARG F388L, a transactivation-deficient mutant, in familial partial lipodystrophy. Diabetes 51, 3586–3590 (2002).
Srinivasan, S. et al. A polygenic lipodystrophy genetic risk score characterizes risk independent of BMI in the diabetes prevention program. J. Endocr. Soc. 3, 1663–1677 (2019).
Privé, F., Arbel, J. & Vilhjálmsson, B. J. LDpred2: better, faster, stronger. Bioinformatics 36, 5424–5431 (2020).
The ARIC investigators. The Atherosclerosis Risk in Communities (ARIC) study: design and objectives. Am. J. Epidemiol. 129, 687–702 (1989).
Ried, J. S. et al. A principal component meta-analysis on multiple anthropometric traits identifies novel loci for body shape. Nat. Commun. 7, 13357 (2016).
Sulc, J. et al. Composite trait Mendelian randomization reveals distinct metabolic and lifestyle consequences of differences in body shape. Commun. Biol. 4, 1–13 (2021).
Després, J.-P. & Lemieux, I. Abdominal obesity and metabolic syndrome. Nature 444, 881–887 (2006).
Makimura, H. et al. Metabolic effects of a growth hormone-releasing factor in obese subjects with reduced growth hormone secretion: a randomized controlled trial. J. Clin. Endocrinol. Metab. 97, 4769–4779 (2012).
Stanley, T. L. et al. Effect of tesamorelin on visceral fat and liver fat in HIV-infected patients with abdominal fat accumulation: a randomized clinical trial. JAMA 312, 380–389 (2014).
Meral, R. et al. ‘Fat Shadows’ from DXA for the qualitative assessment of lipodystrophy: when a picture is worth a thousand numbers. Diabetes Care 41, 2255–2258 (2018).
Laber, S. et al. Discovering cellular programs of intrinsic and extrinsic drivers of metabolic traits using LipocyteProfiler. https://doi.org/10.1101/2021.07.17.452050 (2021).
Sinnott-Armstrong, N. et al. A regulatory variant at 3q21.1 confers an increased pleiotropic risk for hyperglycemia and altered bone mineral density. Cell Metab. 33, 615–628.e13 (2021).
Sudlow, C. et al. UK biobank: an open access resource for identifying the causes of a wide range of complex diseases of middle and old age. PLoS Med. 12, e1001779 (2015).
Littlejohns, T. J. et al. The UK Biobank imaging enhancement of 100,000 participants: rationale, data collection, management and future directions. Nat. Commun. 11, 2624 (2020).
Aschard, H., Vilhjálmsson, B. J., Joshi, A. D., Price, A. L. & Kraft, P. Adjusting for heritable covariates can bias effect estimates in genome-wide association studies. Am. J. Hum. Genet. 96, 329–339 (2015).
Day, F. R., Loh, P.-R., Scott, R. A., Ong, K. K. & Perry, J. R. B. A robust example of collider bias in a genetic association study. Am. J. Hum. Genet. 98, 392–393 (2016).
Bycroft, C. et al. The UK Biobank resource with deep phenotyping and genomic data. Nature 562, 203–209 (2018).
UK10K Consortium. et al. The UK10K project identifies rare variants in health and disease. Nature 526, 82–90 (2015).
1000 Genomes Project Consortium. et al. A global reference for human genetic variation. Nature 526, 68–74 (2015).
Mbatchou, J. et al. Computationally efficient whole-genome regression for quantitative and binary traits. Nat. Genet. 53, 1097–1103 (2021).
Zhou, W. et al. Efficiently controlling for case-control imbalance and sample relatedness in large-scale genetic association studies. Nat. Genet. 50, 1335–1341 (2018).
Loh, P.-R. et al. Efficient Bayesian mixed-model analysis increases association power in large cohorts. Nat. Genet. 47, 284–290 (2015).
Loh, P.-R., Kichaev, G., Gazal, S., Schoech, A. P. & Price, A. L. Mixed-model association for biobank-scale datasets. Nat. Genet. 50, 906–908 (2018).
Winkler, T. W. et al. EasyStrata: evaluation and visualization of stratified genome-wide association meta-analysis data. Bioinformatics 31, 259–261 (2015).
Gamazon, E. R. et al. A gene-based association method for mapping traits using reference transcriptome data. Nat. Genet. 47, 1091–1098 (2015).
Zhu, Z. et al. Integration of summary data from GWAS and eQTL studies predicts complex trait gene targets. Nat. Genet. 48, 481–487 (2016).
GTEx Consortium. Human genomics. The Genotype-Tissue Expression (GTEx) pilot analysis: multitissue gene regulation in humans. Science 348, 648–660 (2015).
Pers, T. H. et al. Biological interpretation of genome-wide association studies using predicted gene functions. Nat. Commun. 6, 5890 (2015).
Fehrmann, R. S. N. et al. Gene expression analysis identifies global gene dosage sensitivity in cancer. Nat. Genet. 47, 115–125 (2015).
Szustakowski, J. D. et al. Advancing human genetics research and drug discovery through exome sequencing of the UK Biobank. Nat. Genet. 53, 942–948 (2021).
Jurgens, S. J. et al. Analysis of rare genetic variation underlying cardiometabolic diseases and traits among 200,000 individuals in the UK Biobank. Nat. Genet. 54, 240–250 (2022).
Li, H. Toward better understanding of artifacts in variant calling from high-coverage samples. Bioinformatics 30, 2843–2851 (2014).
Bailey, J. A. Segmental duplications: organization and impact within the current human genome project assembly. Genome Res. 11, 1005–1017 (2001).
Chang, C. C. et al. Second-generation PLINK: rising to the challenge of larger and richer datasets. GigaScience 4, 7 (2015).
Manichaikul, A. et al. Robust relationship inference in genome-wide association studies. Bioinformatics 26, 2867–2873 (2010).
Zhao, H. et al. CrossMap: a versatile tool for coordinate conversion between genome assemblies. Bioinformatics 30, 1006–1007 (2014).
Karczewski, K. J. et al. The mutational constraint spectrum quantified from variation in 141,456 humans. Nature 581, 434–443 (2020).
Aken, B. L. et al. The Ensembl gene annotation system. Database 2016, baw093 (2016).
Do, R. et al. Exome sequencing identifies rare LDLR and APOA5 alleles conferring risk for myocardial infarction. Nature 518, 102–106 (2015).
Khera, A. V. et al. Diagnostic yield and clinical utility of sequencing familial hypercholesterolemia genes in patients with severe hypercholesterolemia. J. Am. Coll. Cardiol. 67, 2578–2589 (2016).
Khera, A. V. et al. Association of rare and common variation in the lipoprotein lipase gene with coronary artery disease. JAMA 317, 937–946 (2017).
Liu, X., Wu, C., Li, C. & Boerwinkle, E. dbNSFP v3.0: a one-stop database of functional predictions and annotations for human nonsynonymous and splice-site SNVs. Hum. Mutat. 37, 235–241 (2016).
Ng, P. C. & Henikoff, S. SIFT: predicting amino acid changes that affect protein function. Nucleic Acids Res. 31, 3812–3814 (2003).
Adzhubei, I. A. et al. A method and server for predicting damaging missense mutations. Nat. Methods 7, 248–249 (2010).
Chun, S. & Fay, J. C. Identification of deleterious mutations within three human genomes. Genome Res. 19, 1553–1561 (2009).
Schwarz, J. M., Cooper, D. N., Schuelke, M. & Seelow, D. MutationTaster2: mutation prediction for the deep-sequencing age. Nat. Methods 11, 361–362 (2014).
Lee, S., Abecasis, G. R., Boehnke, M. & Lin, X. Rare-variant association analysis: study designs and statistical tests. Am. J. Hum. Genet. 95, 5–23 (2014).
Park, J.-H. et al. Distribution of allele frequencies and effect sizes and their interrelationships for common genetic susceptibility variants. Proc. Natl Acad. Sci. USA 108, 18026–18031 (2011).
Acknowledgements
This work was supported by the Sarnoff Cardiovascular Research Foundation Fellowship (to S.A.), student scholarships from the Dutch Heart Foundation and the Amsterdams Studentenfonds (S.J.J.), grants 1K08HG010155 and 1U01HG011719 (to A.V.K.) from the National Human Genome Research Institute, a grant from the National Institute of Diabetes and Digestive and Kidney Diseases K23DK114551 (to M.S.U.), a Hassenfeld Scholar Award from Massachusetts General Hospital (to A.V.K.), a Merkin Institute Fellowship from the Broad Institute of MIT and Harvard (to A.V.K.), and a sponsored research agreement from IBM Research to the Broad Institute of MIT and Harvard (to P.T.E., A.P., P.B., and A.V.K.).
Author information
Authors and Affiliations
Contributions
S.A., M.W., and A.V.K. conceived and designed the study. S.A., M.W., M.D.R.K., J.S., K.S., and N.D. acquired, analyzed, and interpreted the data. S.A., M.W., and A.V.K. drafted the manuscript. S.A., M.W., M.D.R.K., J.S., H.D., N.D., S.H.C., S.J.J., P.T.E., A.P., K.N., M.C., P.B., M.S.U., and A.V.K. critically revised the manuscript for important intellectual content.
Corresponding author
Ethics declarations
Competing interests
S.A. has served as a scientific consultant to Third Rock Ventures. M.D.R.K., A.P., and P.B. are supported by grants from Bayer AG applying machine learning in cardiovascular disease. P.T.E. receives sponsored research support from Bayer AG and IBM and has consulted for Bayer AG, Novartis, MyoKardia and Quest Diagnostics. A.P. is also employed as a Venture Partner at GV and consulted for Novartis; and has received funding from Intel, Verily and MSFT. M.C. holds equity in Waypoint Bio and is a member of the Nestle Scientific Advisory Board. K.N. is an employee of IBM Research. P.B. serves as a consultant for Novartis. A.V.K. is an employee and holds equity in Verve Therapeutics; has served as a scientific advisor to Amgen, Maze Therapeutics, Navitor Pharmaceuticals, Sarepta Therapeutics, Novartis, Silence Therapeutics, Korro Bio, Veritas International, Color Health, Third Rock Ventures, Illumina, Foresite Labs, and Columbia University (NIH); received speaking fees from Illumina, MedGenome, Amgen, and the Novartis Institute for Biomedical Research; and received a sponsored research agreement from IBM Research. The remaining authors declare no competing interests.
Peer review
Peer review information
Nature Communications thanks Timothy Frayling and the other, anonymous, reviewer(s) for their contribution to the peer review of this work. Peer reviewer reports are available.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Agrawal, S., Wang, M., Klarqvist, M.D.R. et al. Inherited basis of visceral, abdominal subcutaneous and gluteofemoral fat depots. Nat Commun 13, 3771 (2022). https://doi.org/10.1038/s41467-022-30931-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41467-022-30931-2
This article is cited by
-
Bazi Bushen ameliorates age-related energy metabolism dysregulation by targeting the IL-17/TNF inflammatory pathway associated with SASP
Chinese Medicine (2024)
-
The causal relationship between human blood metabolites and the risk of visceral obesity: a mendelian randomization analysis
Lipids in Health and Disease (2024)
-
A new approach to quantify visceral fat via bioelectrical impedance analysis and ultrasound compared to MRI
International Journal of Obesity (2024)
-
Adipose tissue-derived metabolite risk scores and risk for type 2 diabetes in South Asians
International Journal of Obesity (2024)
-
Risk Stratification and Treatment of Obesity for Primary and Secondary Prevention of Cardiovascular Disease
Current Atherosclerosis Reports (2024)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.